Hydroxyurea vs Alternatives Decision Helper
This tool helps compare key features of Hydroxyurea and its alternatives for sickle cell disease. Select a treatment below to see detailed benefits and drawbacks.
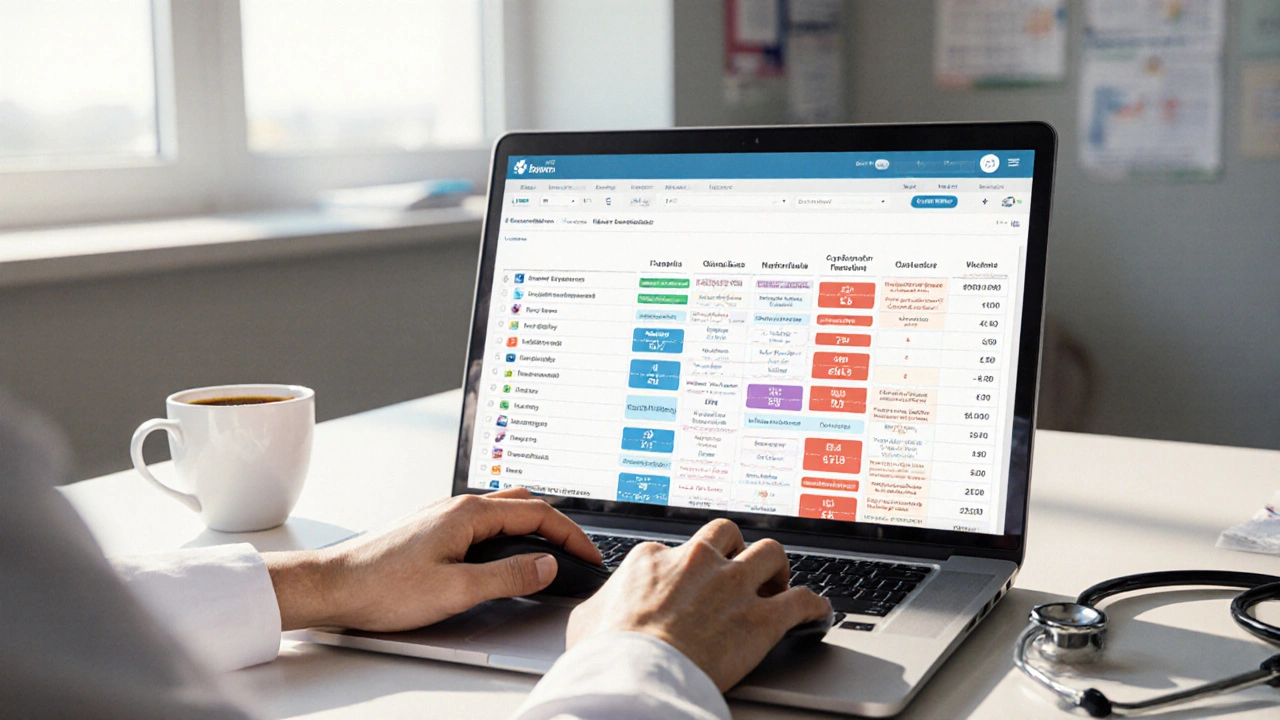
| Drug/Procedure | Mechanism | Route & Frequency | FDA Approval | Main Benefit | Side Effects | Cost Category |
|---|
Key Takeaways
- Hydroxyurea (Hydrea) is the only oral disease‑modifying drug approved for sickle cell disease (SCD) and works by increasing fetal hemoglobin.
- Newer biologics (voxelotor, crizanlizumab) target different disease pathways and can be combined with Hydroxyurea for added benefit.
- Gene‑based therapies and stem‑cell transplant offer curative potential but involve higher cost, stricter eligibility, and more intensive follow‑up.
- Choosing the right option depends on disease severity, age, comorbidities, insurance coverage, and personal preference.
- A side‑by‑side table makes it easier to weigh efficacy, safety, dosing, and cost before deciding.
What Is Hydroxyurea (Hydrea)?
Hydroxyurea is a chemotherapeutic agent that, at low doses, raises fetal hemoglobin (HbF) levels in people with sickle cell disease, reducing vaso‑occlusive crises and the need for blood transfusions. In the UK it is marketed under the brand name Hydrea. First approved for cancer in the 1960s, its sickle‑cell indication arrived in 1998 after clinical trials showed a 44% drop in painful episodes.
The drug is taken orally once daily, usually starting at 15mg/kg and titrated up to the maximum tolerated dose (often 35mg/kg). Monitoring includes blood counts every 2-4weeks during dose escalation and then every 3months.
How Hydroxyurea Works
Hydroxyurea inhibits ribonucleotide reductase, slowing DNA synthesis in rapidly dividing cells. In sickle cell patients the side effect of mild bone‑marrow suppression triggers stress erythropoiesis, which in turn boosts production of HbF. Fetal hemoglobin does not sickle, so red cells become more flexible and less likely to clog small vessels.
Beyond HbF, the drug also reduces white‑blood‑cell count and adhesion molecule expression, lowering the inflammatory cascade that fuels sickle‑cell complications.
Benefits and Drawbacks of Hydroxyurea
- Pro: Proven to lower pain‑crisis frequency by 30‑50% and decrease hospital admissions.
- Pro: Oral administration-no infusion centers needed.
- Pro: Relatively low cost compared with biologics or gene therapy.
- Con: Myelosuppression can cause neutropenia or thrombocytopenia; regular labs are mandatory.
- Con: Some patients experience leg ulcers or gastrointestinal upset.
- Con: Effectiveness varies; about 20‑30% of patients achieve only modest HbF rises.
What Are the Main Alternatives?
Because Hydroxyurea does not work for everyone, several newer agents have entered the market. Each targets a different mechanism-either improving red‑cell oxygen affinity, blocking adhesion, or correcting the genetic defect.
- L‑glutamine (an amino‑acid supplement that reduces oxidative stress in red cells, approved by the FDA in 2017 for SCD)
- Voxelotor (an oral hemoglobin‑oxygen‑affinity modifier that stabilises the oxygenated form of hemoglobin, FDA‑approved 2019)
- Crizanlizumab (a monoclonal antibody that blocks P‑selectin, reducing vaso‑occlusion; approved 2020)
- Gene therapy (e.g., Lenti‑globin, CRISPR/Cas9) (single‑dose approaches that add or edit the β‑globin gene to raise HbF permanently)
- Allogeneic stem‑cell transplant (the only proven curative option, replacing the patient’s marrow with a donor’s healthy cells)
Side‑by‑Side Comparison
| Drug/Procedure | Mechanism | Route & Frequency | FDA Approval (US) | Main Benefit | Significant Side Effects | Relative Cost* |
|---|---|---|---|---|---|---|
| Hydroxyurea (Hydrea) | Increases HbF via ribonucleotide‑reductase inhibition | Oral, once daily | 1998 (SCD) | ↓ pain crises, ↓ transfusions | Myelosuppression, leg ulcers, GI upset | Low |
| L‑glutamine | Reduces oxidative stress in red cells | Oral, twice daily | 2017 | Modest ↓ hospitalizations | Flatulence, mild nausea | Low‑moderate |
| Voxelotor | Increases hemoglobin‑oxygen affinity, prevents polymerisation | Oral, once daily | 2019 | ↑ hemoglobin levels, ↓ hemolysis | Headache, diarrhea | Moderate |
| Crizanlizumab | Anti‑P‑selectin monoclonal antibody, blocks cell adhesion | IV infusion, every 2 weeks | 2020 | ↓ vaso‑occlusive crises | Infusion reactions, pain at site | High |
| Gene therapy (Lenti‑globin/CRISPR) | Introduces functional β‑globin or re‑activates γ‑globin genes | Single infusion/conditioned transplant | 2022 (early‑phase) | Potential cure, sustained HbF | Conditioning regimen toxicity, unknown long‑term risks | Very high |
| Allogeneic stem‑cell transplant | Replaces defective marrow with donor’s healthy stem cells | Hospital‑based, one‑time procedure | 1970s (experimental), now standard for select cases | Curative | Graft‑vs‑host disease, transplant‑related mortality | Very high |
*Cost categories are relative to the UK NHS context in 2025 and exclude indirect expenses such as travel for infusions.
How to Choose the Right Option
Deciding whether to stay on Hydroxyurea or switch to another therapy involves a mix of clinical data and personal circumstances. Below is a practical checklist you can run through with your hematologist.
- Disease severity: Frequent crises (>3 per year) or chronic organ damage usually trigger escalation.
- Response to Hydroxyurea: If HbF rise < 20% after 6months, consider adding or swapping.
- Age and growth considerations: Children <5years often start with Hydroxyurea; adults may be eligible for gene therapy trials.
- Comorbidities: Renal impairment limits certain drugs; liver disease may affect metabolism.
- Access & cost: IV biologics require infusion centres; gene therapy is limited to specialist centres.
- Patient preference: Some patients dislike frequent blood draws, others avoid pills.
Use this matrix to score each option (1=poor, 5=excellent) and discuss the total with your care team.
Practical Tips for Managing Hydroxyurea
Even if you decide Hydroxyurea remains your best choice, the following habits improve safety and effectiveness:
- Schedule CBC labs on the same day each month; set a phone reminder.
- Take the dose at the same time daily-preferably with food to reduce stomach upset.
- Keep a pain‑crisis diary (date, severity, meds). This helps the doctor see trends.
- Stay hydrated; dehydration worsens sickling regardless of therapy.
- If you notice persistent bruising or infections, call your clinic right away.
Future Landscape
Research pipelines are bustling. Late‑stage trials of next‑gen CRISPR‑based editing promise a one‑time cure with fewer conditioning drugs. Meanwhile, oral agents that combine HbF induction with anti‑adhesion (dual‑acting molecules) are in PhaseIII. By 2030, the standard of care may shift from chronic drug regimens to curative gene‑editing for most patients.
Frequently Asked Questions
Can I stop Hydroxyurea if I start a newer drug?
Most clinicians recommend a gradual taper rather than an abrupt stop, especially if you’ve been on Hydroxyurea for years. This avoids a sudden drop in HbF and reduces the risk of rebound crises. Discuss a transition plan with your hematologist.
Is Hydroxyurea safe during pregnancy?
Hydroxyurea is classified as pregnancy‑category D in the US and is generally avoided in the UK unless the benefits clearly outweigh the risks. Women planning pregnancy are usually switched to alternate therapies or observed closely.
How does Crizanlizumab differ from Hydroxyurea?
Crizanlizumab targets P‑selectin, a molecule that makes sickled cells stick to blood‑vessel walls. Hydroxyurea raises HbF, making cells less likely to sickle. Because they act on separate pathways, doctors sometimes use them together for additive benefits.
What monitoring is required for gene therapy?
After a gene‑editing procedure, patients need regular blood work for the first 6months, then quarterly checks for at least 5years to monitor vector integration, hemoglobin levels, and any off‑target effects.
Is stem‑cell transplant still the best curative option?
For patients with a matched sibling donor, transplant offers the highest cure rate (>90%). However, the risk of graft‑vs‑host disease and transplant‑related mortality means it’s reserved for severe cases or when other options fail.
Next Steps
1. Schedule a review appointment with your hematology team.
2. Bring recent CBC results, a pain‑crisis log, and this comparison table.
3. Discuss eligibility for newer agents or clinical trials based on your age and disease status.
4. Decide whether to continue Hydroxyurea, add a second‑line drug, or explore curative options.
Remember, the best choice balances medical evidence with what fits your life. Keep the conversation open and revisit the plan every 12months.




Comments
Phoebe Chico
October 5, 2025 AT 12:18 PMWhen we stand at the crossroads of chemistry and compassion, Hydroxyurea emerges as a quiet hero, a humble pill that whispers promises of fewer crises and brighter tomorrows. Its mechanism, a gentle tug on the ribonucleotide‑reductase, awakens the dormant fetal hemoglobin that once cradled us in the womb. This reawakening turns the sickle‑shaped enemies into pliable, flexible carriers of life’s oxygen. Imagine a world where pain crises tumble like dominoes, one after another, succumbing to the subtle power of a daily dose. The data sings-a 30‑50% plunge in vaso‑occlusive episodes, a chorus of reduced transfusions echoing in hospital corridors. Oral administration, a single daily ritual, sidesteps the tyranny of infusion centers and the cold sterility of IV lines. Cost, a modest whisper in the cacophony of modern therapeutics, keeps Hydroxyurea within reach for many, a democratic savior in a market of extravagance. Yet, the journey is not without shadows; myelosuppression can stalk the unwary, demanding vigilant blood counts and a steady hand. Leg ulcers and gastrointestinal grumbles sometimes scar the path, reminders that even miracles bear a price. Approximately a fifth to a third of patients glimpse only modest HbF rises, a reminder that biology guards its own secrets. Still, the collective chorus of clinicians, patients, and families raise a toast to its proven legacy since 1998. In the grand tapestry of sickle cell care, Hydroxyurea threads a line of hope, resilience, and accessible science. It teaches us that sometimes the most profound changes begin with a single, unassuming tablet. Let us honor its place, not as a relic, but as a living bridge between past discoveries and future cures. And as we stand, gazing toward gene therapy’s horizon, we must not abandon the steadfast companion that has steadied countless lives for decades.
Larry Douglas
October 11, 2025 AT 09:38 AMHydroxyurea's pharmacodynamics are well‑documented its impact on HbF elevation is dose‑dependent however routine monitoring is essential to avoid cytopenias which can be detrimental especially in patients with pre‑existing marrow stress
Michael Stevens
October 17, 2025 AT 06:58 AMHey folks, just wanted to add that Hydroxyurea works best when patients stick to the titration schedule and keep up with their labs. It’s a team effort between you, your hematologist, and the lab techs!
Ann Campanella
October 23, 2025 AT 04:18 AMHydroxyurea is cheap.
Desiree Tan
October 29, 2025 AT 00:38 AMListen, the real strength of Hydroxyurea is that it’s oral – no need to schedule bi‑weekly infusions that ruin your weekend plans. Plus, the side‑effect profile, while not nonexistent, is manageable with regular blood work. If you’re on the fence, weigh the daily pill against the hassle and expense of biologics; you’ll often find the pill wins the cost‑benefit battle.
Andrea Dunn
November 3, 2025 AT 21:58 PMSure, but remember the pharma giants push Hydroxyurea because they own the patents on the newer gene‑editing tech. They want you to think it’s the only affordable option while they line their pockets with CRISPR subsidies. 👀
Erin Johnson
November 9, 2025 AT 19:18 PMLet’s be crystal clear: Hydroxyurea isn’t a miracle cure, but calling it “just a cheap pill” is a disservice. Its real value lies in reducing pain crises, which translates to fewer ER visits and a better quality of life. The trade‑off? Regular lab monitoring and the occasional leg ulcer. For many patients, that’s a small price for freedom from constant pain. If you think the cost is negligible, you’ve probably never faced a hospital admission for a vaso‑occlusive event. So, respect the drug, respect the monitoring, and keep pushing for better therapies alongside it.
Rica J
November 15, 2025 AT 16:38 PMi love how the table makes it super easy to see the diff. hydroxyurea is def the most budget friendly option but u still need 2-4wk labs. l‑glutamine is kinda meh for me, just a little tummy upset. voxelotor feels ok but its price tag is steep. overall, i think start with hydroxyurea unless u cant tolerate it.
Linda Stephenson
November 21, 2025 AT 13:58 PMGreat breakdown! I’d add that patient preference matters a lot – some folks hate taking daily meds, so they might opt for an infusion despite the cost. Also, checking insurance coverage early can save a lot of headache later.
Sunthar Sinnathamby
November 27, 2025 AT 11:18 AMFolks, if you’re still on the fence, think about your lifestyle. Hydroxyurea’s once‑daily pill fits a busy schedule, while the IV drugs demand regular trips to the clinic. The freedom to travel, work, or just binge‑watch your favorite series without scheduling infusions is priceless. And hey, the data on reducing admissions is solid – fewer sick days, more life days.
Catherine Mihaljevic
December 3, 2025 AT 08:38 AMHonestly the whole "new drugs are better" narrative is just pharma hype. Every time a new big‑ticket therapy hits the market, they hide the long‑term risks. Look at the infusion reactions – they’re not "minor".
Michael AM
December 9, 2025 AT 05:58 AMTotally get the concerns, but the monitoring protocols for Hydroxyurea are well‑established and not that burdensome if you’re organized.
Rakesh Manchanda
December 15, 2025 AT 03:18 AMFrom an academic standpoint, the mechanistic elegance of Hydroxyurea-modulating ribonucleotide reductase to induce fetal hemoglobin-is a testament to translational science. Yet, the therapeutic horizon now expands toward genome editing, promising a paradigm shift.
Erwin-Johannes Huber
December 21, 2025 AT 00:38 AMIndeed, the scientific community should celebrate both incremental advances like Hydroxyurea and the bold strides of gene therapy. Collaboration will drive the best outcomes.
Tim Moore
December 26, 2025 AT 21:58 PMIn summation, the selection of therapy must be anchored in rigorous clinical evidence, individual patient phenotype, and socioeconomic considerations. Hydroxyurea remains a cornerstone, yet the therapeutic armamentarium is diversifying contemporaneously.
Erica Ardali
January 1, 2026 AT 19:18 PMAh, the ever‑dazzling drama of medical choices-hydroxyurea, the humble workhorse, versus the glittering new biopharma toys. One must ask: is the sparkle worth the cost? 🎭
Justyne Walsh
January 7, 2026 AT 16:38 PMSure, let’s all ignore the fact that the “new” drugs are just a way for big pharma to keep profits soaring while patients chase shiny objects. Classic.
Callum Smyth
January 13, 2026 AT 13:58 PMLet's keep it constructive: each option has its place, and a shared decision‑making approach empowers patients to choose what aligns with their values and life circumstances.