When you’ve had a severe reaction to a drug, your body isn’t just saying "no" to that one pill-it’s screaming about the whole family. That’s why doctors often tell you to avoid every drug in that class. But here’s the truth: not every severe reaction means you need to avoid everything in the family. Too many people are told to skip entire groups of medications based on a single bad experience, only to end up with fewer treatment options, longer hospital stays, or worse outcomes. The key isn’t just avoiding drugs-it’s knowing which ones you really need to steer clear of.
What Counts as a Severe Drug Reaction?
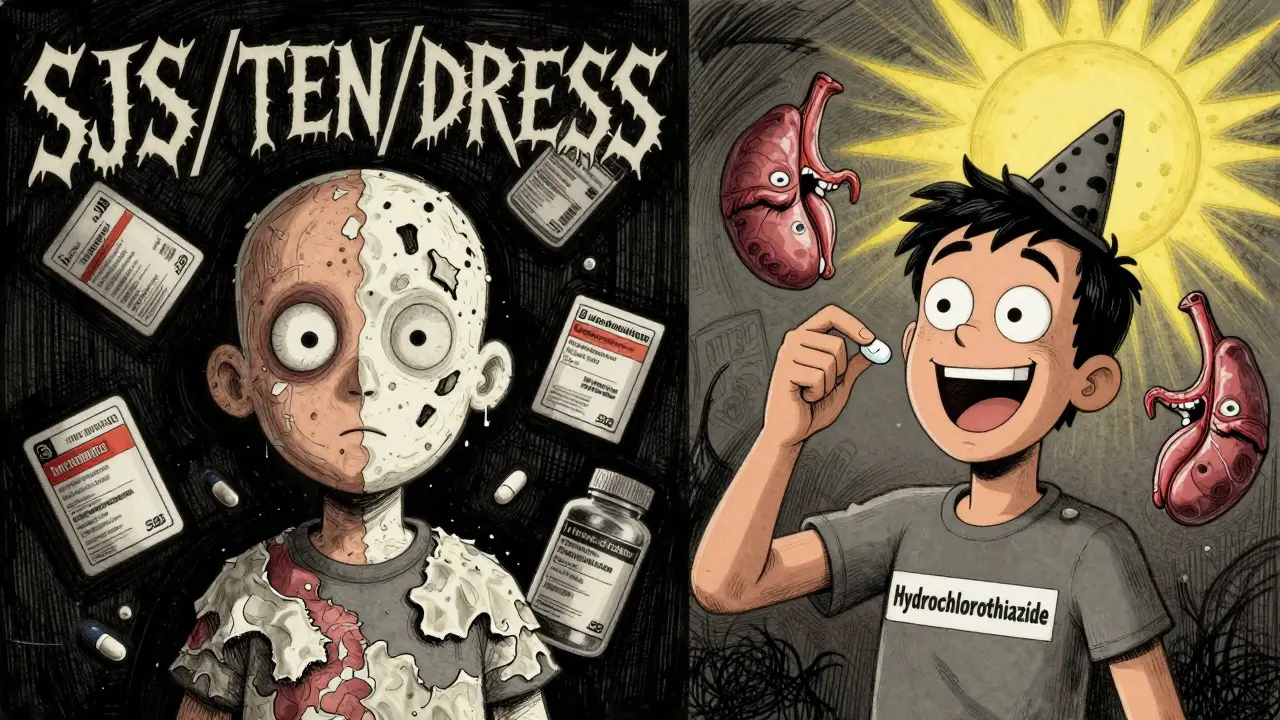
A severe drug reaction isn’t just a rash or upset stomach. The FDA defines it as something that’s life-threatening, requires hospitalization, causes lasting disability, or leads to birth defects. In real terms, that means reactions like anaphylaxis-where your throat swells and you can’t breathe-or rare but deadly conditions like Stevens-Johnson syndrome, where your skin starts peeling off, or DRESS, which triggers organ failure along with a raging rash.
These aren’t common. But when they happen, they’re serious. About 1.3 million people in the U.S. end up in the emergency room every year because of bad drug reactions, and 350,000 are admitted to the hospital. Antibiotics are the biggest culprit-especially penicillin and sulfa drugs. But here’s what most people don’t realize: most drug reactions aren’t allergic. Around 80-90% are predictable side effects, like nausea from NSAIDs or dizziness from blood pressure meds. Those don’t mean you need to avoid the whole class.
True Allergies vs. Side Effects: The Big Difference
If you broke out in hives 30 minutes after taking penicillin and your face swelled up, that’s a true IgE-mediated allergic reaction. Your immune system saw the drug as an invader and went to war. That’s rare-only about 10% of people labeled "penicillin allergic" actually have this kind of reaction. The rest? They had a non-allergic rash, maybe from a virus they had at the same time, or a mild reaction that didn’t involve their immune system.
Same with sulfa drugs. If you got Stevens-Johnson syndrome after taking Bactrim, you’re in the small group that needs to avoid all sulfa antibiotics forever. But if you just got a mild rash from sulfamethoxazole and it went away after stopping the drug, you might not need to avoid all sulfa drugs. The same goes for NSAIDs. If you get stomach bleeding from ibuprofen, switching to celecoxib (a COX-2 inhibitor) might be fine. The problem isn’t the class-it’s the mechanism.
Drug Families That Almost Always Need Avoidance
There are some classes where avoiding the whole group is non-negotiable. These are the ones that cause severe cutaneous adverse reactions (SCARs). If you’ve had:
- Stevens-Johnson syndrome (SJS)
- Toxic epidermal necrolysis (TEN)
- Drug reaction with eosinophilia and systemic symptoms (DRESS)
then you need to avoid the entire drug family. TEN alone kills 30-50% of people who get it. And 95% of all TEN cases come from just six drug classes: antibacterial sulfonamides, anticonvulsants like carbamazepine, allopurinol, NSAIDs, nevirapine, and corticosteroids. Once you’ve had one of these reactions, the risk of it happening again is too high. No second chances.
For sulfonamide antibiotics, cross-reactivity is about 10%. That means if you reacted to Bactrim, you might also react to Septra or sulfasalazine. But you can still take sulfa-based diuretics like hydrochlorothiazide-those are chemically different and rarely cause the same reaction. It’s not about the word "sulfa"-it’s about the specific molecule.
Penicillin: The Most Misunderstood Allergy
Penicillin is the most common drug allergy label in the U.S.-but up to 95% of people who say they’re allergic to it aren’t. Many got the label as kids after a rash that wasn’t even caused by the drug. Years later, they’re still avoiding all penicillins, cephalosporins, and even carbapenems, even though cross-reactivity between penicillin and cephalosporins is only 0.5-6.5%, and mostly limited to older generations.
Studies show that if you get tested-through skin testing or an oral challenge under supervision-70-85% of people with a penicillin allergy label can safely take it. In one case, a woman avoided all antibiotics for 20 years because she got a rash as a child. After testing, she was cleared to take amoxicillin for a sinus infection. No reaction. No problem.
Doctors are starting to catch on. By 2023, 87% of academic medical centers in the U.S. had formal penicillin de-labeling programs. If you think you’re allergic to penicillin, ask for a referral to an allergist. You might be able to get back a whole class of safe, effective, and cheaper antibiotics.
When You Can Still Use Drugs in the Same Family
Not every reaction means total avoidance. Here’s how to think about it:
- Statin-induced muscle pain? Only 10-15% of people react to more than one statin. Switching from atorvastatin to rosuvastatin often works fine.
- GI upset from aspirin? If it’s just stomach irritation, try enteric-coated aspirin or switch to a different NSAID like naproxen. But if you get asthma attacks or nasal polyps after aspirin, you likely have aspirin-exacerbated respiratory disease-then you need to avoid all NSAIDs.
- Rash from amoxicillin? If it’s a non-itchy, flat rash that shows up days after starting the drug, it’s probably not an allergy. It’s common in kids with mono and doesn’t mean you can’t take penicillin again.
The rule of thumb? If your reaction was immune-driven-hives, swelling, trouble breathing, blistering skin-avoid the class. If it was a predictable side effect-nausea, dizziness, headache, mild rash-it’s often safe to try another drug in the same family.

What to Do After a Severe Reaction
After a bad reaction, don’t just take the doctor’s word for it. Ask these five questions:
- What exactly happened? (Hives? Low blood pressure? Skin peeling?)
- When did it happen? (Minutes after taking it? Days later?)
- Was it treated in the ER or hospital?
- Is this a known cross-reactive drug family?
- Can I get tested or do a drug challenge?
Make sure your allergy is documented clearly in your medical record-not just as "penicillin allergy," but as "anaphylaxis to amoxicillin, 2021." Use standardized terms like SNOMED CT codes so other doctors understand the severity. Poor documentation leads to 23% of allergy alerts being ignored in hospitals, putting patients at risk.
Also, carry a medical alert bracelet if you’ve had anaphylaxis or SCARs. And ask for an epinephrine auto-injector if you’re at risk of another reaction. About 90% of specialists recommend it for anaphylaxis survivors.
The Future: Better Testing, Fewer Unnecessary Avoidances
Technology is catching up. In 2022, the FDA approved the first component-resolved diagnostic test for drug allergies-ImmunoCap Specific IgE. It’s way more accurate than old skin tests, cutting false positives from 40% down to 11%. Genetic testing is also helping. If you carry the HLA-B*57:01 gene, you’re at extreme risk for a deadly reaction to abacavir (an HIV drug). Test for it first, and you can safely give the drug to 95% of people who were previously avoided.
AI tools like IBM Watson for Drug Safety are now helping hospitals predict which patients are likely to have false allergy labels. In one trial, it reduced unnecessary avoidance by 41%. That’s huge. More people are getting tested, more doctors are asking the right questions, and more patients are getting the right meds.
But the biggest change? Mindset. We’re moving from "avoid everything" to "avoid what’s proven dangerous." That’s not just safer-it’s smarter. It means fewer missed treatments, fewer hospitalizations, and better outcomes.
Bottom Line: Don’t Assume, Find Out
If you’ve had a severe drug reaction, you’re right to be cautious. But you’re not right to assume you need to avoid the whole family. The difference between life and death isn’t always in the drug-it’s in the diagnosis. Ask for testing. Get your allergy properly labeled. Don’t let a label from 10 years ago keep you from the best treatment today.
There’s no shame in being allergic. But there’s real danger in being mislabeled. You deserve the right medication-not just the safest one on paper, but the one that actually works for you.







Comments
Anna Weitz
December 26, 2025 AT 12:26 PMSo you're telling me my kid's rash from amoxicillin at age 4 doesn't mean he can never have penicillin again? Holy shit. My whole family's been avoiding antibiotics like they're poison for 15 years because of that one time. I'm calling the allergist Monday.
Liz MENDOZA
December 27, 2025 AT 08:16 AMThis is the kind of post that saves lives. I'm a nurse and I've seen so many patients denied life-saving meds because of a vague allergy label in their chart. One woman avoided all NSAIDs because she got a stomach ache once-turned out she had ulcers from stress, not the drug. Doctors need to stop being lazy with these labels. Thank you for this.
Olivia Goolsby
December 29, 2025 AT 04:17 AMOhhhh so now the pharmaceutical companies are secretly manipulating our immune systems through vague allergy labels so we keep buying expensive new drugs?? And the FDA approved some "component-resolved diagnostic test"?? That's just a fancy name for a blood test they're forcing us to pay for while they quietly retire the old penicillin skin test that actually worked for decades!! You think they don't profit when you're stuck with 500-dollar alternatives because you were told to avoid penicillin for no reason?? They're not trying to help you-they're trying to lock you into their patented, overpriced, side-effect-laden "next-gen" drugs!! And don't even get me started on the HLA-B*57:01 gene testing-what if that's just another way to screen people for insurance discrimination?? This isn't medicine-it's corporate control disguised as science!!
Alex Lopez
December 29, 2025 AT 19:10 PMExcellent breakdown. Though I must say, the fact that 95% of penicillin "allergies" are false positives is both hilarious and terrifying. I once had a patient who refused all beta-lactams because she "got a rash once in college"-turned out she had mono. She cried when we confirmed she could take amoxicillin. Also, thank you for mentioning epinephrine auto-injectors. So many patients are discharged from ERs after anaphylaxis without one. It's not paranoia-it's preparedness. Sarcasm aside: this is critical information.
Gerald Tardif
December 30, 2025 AT 08:03 AMMan. I used to be the guy who’d say "avoid everything" after a bad reaction. Then my sister got DRESS from allopurinol. We thought she’d never take another med again. But after testing? Turns out she’s fine with sulfa diuretics. Now she’s on hydrochlorothiazide and her blood pressure’s stable. I used to think "sulfa" meant danger. Now I know it’s about the molecule. That’s the difference between fear and science.
Monika Naumann
December 30, 2025 AT 15:11 PMIt is deeply concerning that Western medical institutions are so eager to discard traditional cautionary practices in favor of unproven diagnostic technologies. In our country, we respect the body’s wisdom-when it reacts severely, it is a sign from nature that the substance is incompatible. To suggest that one can simply "test" and re-enter the same class of drugs is to ignore the spiritual and energetic imbalance caused by synthetic chemicals. This is not progress. This is arrogance dressed in white coats.
Elizabeth Ganak
December 30, 2025 AT 16:58 PMAs someone from India, I’ve seen this firsthand. My aunt got a rash on amoxicillin and was told never to take antibiotics again. She ended up with a kidney infection that nearly killed her because they gave her something way more expensive and less effective. I showed her this article-she’s going to get tested next week. Thank you for putting this out there.
Nicola George
December 31, 2025 AT 18:24 PMSo let me get this straight-after a decade of being told "never again" for a mild rash, I could’ve been taking ibuprofen this whole time? And now I’m supposed to be grateful because some AI told me I’m not allergic? Cool. I’ll take the epinephrine injector, the 3-hour allergy test, and the $800 bill. Thanks for the optimism, but I’ve been burned by this system too many times to trust it. I’ll just keep avoiding everything. At least I’m alive.
Raushan Richardson
December 31, 2025 AT 19:27 PMTHIS. I’ve been telling my friends this for years. If you got a rash after penicillin and you’re 30 now? You’re probably fine. Don’t let a childhood mistake cost you your health later. I got my label removed last year-now I can take the cheap antibiotics instead of the $$$ ones. My wallet and my doctor both thank me.
Robyn Hays
January 2, 2026 AT 11:06 AMIt’s wild how much we’ve been conditioned to fear drug classes like they’re cursed bloodlines. I used to think "sulfa" meant danger, but now I know hydrochlorothiazide and Bactrim are chemically different as apples and oranges. And the HLA-B*57:01 gene thing? Mind-blowing. We’re not just treating symptoms anymore-we’re decoding why our bodies react. This isn’t just medicine. It’s personalized survival.
Liz Tanner
January 4, 2026 AT 00:17 AMWell-written, accurate, and urgently needed. I’ve worked in primary care for 18 years, and the number of patients mislabeled with drug allergies is staggering. I’ve had patients refuse penicillin for UTIs because they had a rash at age five. I’ve had patients avoid NSAIDs for arthritis because they got a stomachache once. The documentation is often vague, outdated, or outright wrong. Please, if you have a drug allergy label-ask for a review. Your future self will thank you.