What Really Causes a Gout Attack?
It’s not just about eating too much steak or drinking too much beer. A gout attack happens when tiny, sharp crystals of monosodium urate form inside your joints-usually the big toe, but also knees, ankles, or fingers. These crystals don’t appear out of nowhere. They form because there’s too much uric acid in your blood. That number? 6.8 mg/dL is the tipping point. Once you go over it, uric acid starts turning into crystals. And once those crystals are there, your body sees them as invaders.
Your immune system goes into overdrive. Special cells called macrophages grab those crystals and trigger a chain reaction. One key player is the NLRP3 inflammasome, which kicks off a flood of interleukin-1β, a powerful inflammatory signal. That’s what makes your joint red, swollen, hot, and painfully tender. It’s not the uric acid itself hurting you-it’s your body’s reaction to the crystals.
Here’s the twist: most people with high uric acid never get gout. And some people with gout have uric acid levels that aren’t sky-high. What matters most is whether those crystals have formed and stayed in your joints. Once they’re there, even small changes can set off an attack.
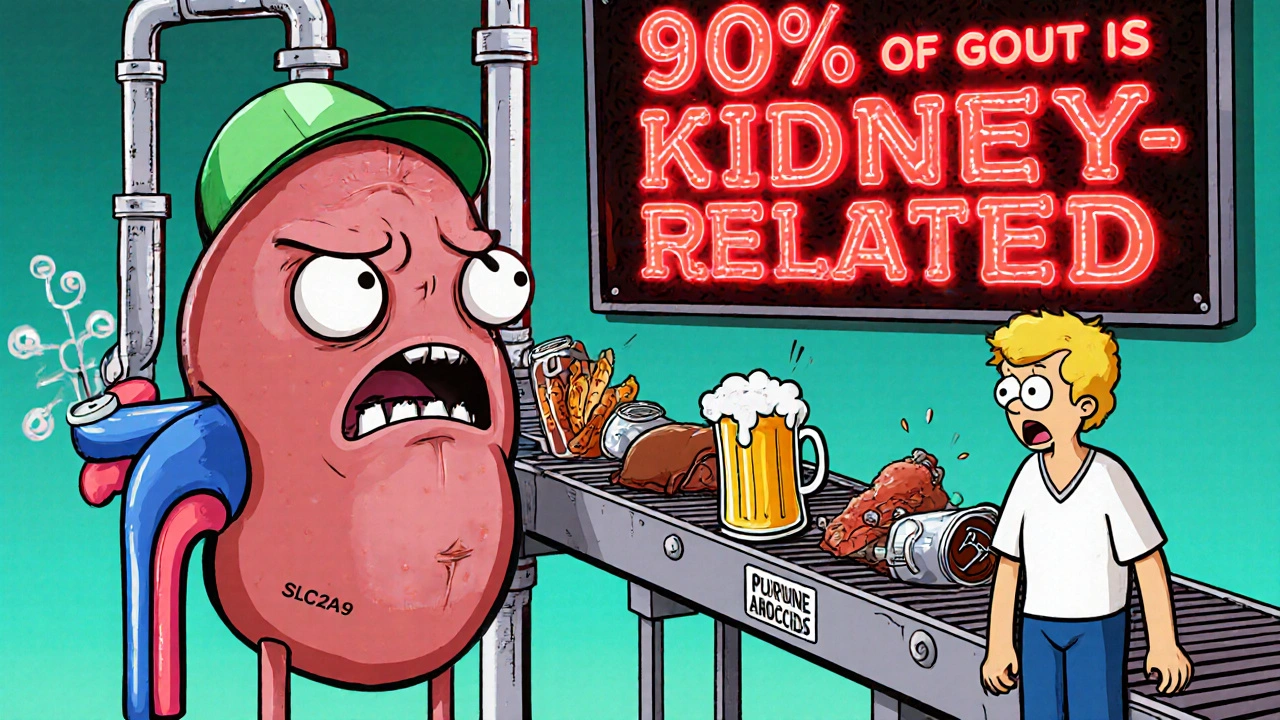
Why Do You Have Too Much Uric Acid?
Ninety percent of gout cases come from your kidneys not flushing out enough uric acid. It’s not that you’re making too much-it’s that your body won’t let it leave. This is often genetic. Genes like SLC2A9 and SLC22A12 control how uric acid moves in and out of your kidneys. If these genes don’t work right, uric acid gets reabsorbed instead of excreted.
Less than 10% of cases are from overproduction. That usually happens with conditions like certain blood cancers or after intense cell turnover. But even then, diet plays a role. Organ meats like liver or kidneys have 300-500 mg of purines per 3-ounce serving. Purines break down into uric acid. So eating a big plate of sweetbreads or anchovies can spike your levels fast.
Drinks matter too. Beer doesn’t just have alcohol-it’s packed with purines. A 12-ounce serving can add 5-10 grams of purines to your system. And sugary sodas? They’re worse than you think. Fructose in high-fructose corn syrup breaks down in your liver and drains ATP, which then turns into uric acid. Studies show drinking one sugary soda a day raises your gout risk by 20-30%.
What Triggers a Sudden Attack?
You can have crystals sitting in your joint for years without trouble. Then, something changes-and boom, you’re in agony. It’s not always food or drink. Sometimes, it’s something simple:
- Dehydration: When you’re not drinking enough water, your urine output drops below 1.5 liters a day. That means uric acid concentrates in your blood and joints.
- Joint injury: Even a minor bump or twist can shake loose crystals from a tophus (a lump of crystals under the skin) and trigger inflammation.
- Rapid changes in uric acid: This is the biggest surprise for most people. Starting a urate-lowering drug like allopurinol can cause a flare. Why? Because your body sees the sudden drop in uric acid as a threat. The crystals start to dissolve, and your immune system reacts. That’s why you need anti-inflammatory protection when you start treatment.
- Alcohol, especially beer: A daily 12-ounce beer raises your risk by 49%. Spirits raise it by 15%. Wine? Not so much. The purines in beer are the main culprit.
Here’s something most people don’t realize: lowering uric acid doesn’t stop an attack that’s already happening. In fact, it can make it worse. That’s why you don’t start allopurinol during a flare. You treat the pain first, then begin long-term therapy once it’s calm.
How Do You Treat an Active Gout Attack?
When the pain hits, you need fast relief. There are three main options, all backed by the American College of Rheumatology:
- NSAIDs: Indomethacin 50 mg three times a day for 3-5 days is common. Ibuprofen or naproxen work too. But if you have kidney problems or stomach ulcers, these aren’t safe.
- Colchicine: The old-school choice. You take 0.6 mg every hour until symptoms improve or you get diarrhea (usually 3-4 doses). For ongoing use, it’s just 0.6 mg once or twice daily. Side effects? Diarrhea in 10-20% of people. It’s not fun, but it works.
- Corticosteroids: If you can’t take NSAIDs or colchicine, prednisone 30-40 mg daily for 5 days, then slowly tapered, is very effective. You can also get a joint injection directly into the affected area.
Ice, rest, and elevation help too. But pills are what stop the fire. Don’t wait. The sooner you start treatment, the shorter the attack.
Long-Term Gout Management: It’s Not Optional
Many people stop their medication when they feel better. That’s a mistake. Gout isn’t cured when the pain goes away. It’s managed when your uric acid stays low.
The goal? Keep your serum uric acid below 6 mg/dL. For people with tophi (visible lumps of crystals), aim for 5 mg/dL. Why? Because below 5 mg/dL, crystals start dissolving. Studies show that after 12 months at this level, 70% of people see their tophi disappear. At 6 mg/dL? Only 30% do.
First-line drug? Allopurinol. Start at 100 mg daily. Increase by 100 mg every 2-5 weeks until you hit your target. Most people need 300-600 mg daily. Some need up to 800 mg. Don’t rush. Check your uric acid every 2-5 weeks until it’s stable.
If allopurinol doesn’t work or causes a rash (rare, but serious), try febuxostat. It’s taken once daily, 40-80 mg. For people with healthy kidneys, probenecid can help the kidneys flush out more uric acid. But it won’t work if your kidneys are already damaged.
Here’s the rule: Never start urate-lowering therapy without anti-inflammatory cover. Low-dose colchicine (0.6 mg once or twice daily) reduces flare risk by 50-75% during the first 6 months. This isn’t optional. It’s standard care.
Diet and Lifestyle: What Actually Helps
You don’t need to eliminate all meat or go vegan. But smart changes make a big difference:
- Drink water: Aim for 2-3 liters a day. More urine means less crystal formation.
- Choose low-fat dairy: One serving a day (like a cup of milk or yogurt) cuts your risk by 43%. The proteins in milk help your kidneys excrete uric acid.
- Avoid beer and sugary drinks: Beer is the worst. Skip the soda. Diet soda? Fine.
- Limit red meat and shellfish: Organ meats, anchovies, sardines, mussels-these are high-risk. Chicken and turkey? Moderate. Tofu and legumes? Safe.
- Maintain a healthy weight: Losing 10% of your body weight can drop uric acid by 1.5 mg/dL.
And don’t forget: alcohol isn’t just about purines. It also dehydrates you and stresses your liver. That double hit makes it a major trigger.
What Happens If You Stop Taking Your Medicine?
Stopping allopurinol or febuxostat for even a few weeks? Your uric acid climbs back to where it was before-fast. Within 2-4 weeks, crystals start reforming. Then, another attack comes. And the next one might be worse.
People often think: “I haven’t had a flare in 6 months. I don’t need this anymore.” But gout doesn’t go away. The crystals are still there. You’re just in a quiet phase. Stopping treatment is like turning off the fire alarm but leaving the smoke in the house.
Adherence is the biggest challenge. Many patients stop because they don’t understand the difference between treating pain and treating the disease. Your doctor isn’t giving you allopurinol to stop your toe from hurting today. They’re giving it to stop you from needing a wheelchair in 5 years.
What’s New in Gout Treatment?
Science is moving fast. The latest research isn’t just about lowering uric acid-it’s about stopping the inflammation at its source.
Drugs that block the NLRP3 inflammasome, like dapansutrile, are in phase III trials. In early studies, they cut flare duration by 40% compared to placebo. This could be the first treatment that targets the actual cause of pain, not just the symptom.
Another area? Gut health. Early studies suggest certain probiotics might help your body break down purines before they turn into uric acid. One trial showed a 10-15% drop in uric acid after 8 weeks of specific probiotic strains. It’s not a replacement for medication, but it could help.
And imaging? Doctors now use ultrasound and dual-energy CT scans to see crystals in joints before they cause pain. That means we can start treatment earlier-even before the first attack.
Key Takeaways
- Gout is caused by uric acid crystals, not high uric acid alone.
- 90% of cases are from kidneys not excreting enough uric acid-not from diet.
- Alcohol (especially beer) and sugary drinks are major triggers.
- Never start urate-lowering drugs during an attack-treat the flare first.
- Always take colchicine for 6 months when starting allopurinol or febuxostat.
- Target uric acid below 6 mg/dL, ideally 5 mg/dL, for life.
- Stopping medication causes uric acid to rebound quickly-flares return.
- Low-fat dairy and water are your best dietary allies.
- New drugs targeting inflammation (not just uric acid) are on the horizon.
Frequently Asked Questions
Can gout be cured?
Gout can’t be cured, but it can be fully controlled. With consistent urate-lowering therapy and lifestyle changes, most people stop having attacks entirely. Crystals dissolve over time, tophi shrink, and joint damage halts. But if you stop treatment, the disease comes back. It’s a lifelong condition that requires ongoing management-not a one-time fix.
Is it safe to take allopurinol long-term?
Yes, for most people. Allopurinol has been used safely for over 50 years. The main risk is a rare allergic reaction called allopurinol hypersensitivity syndrome, which occurs in 0.1-0.4% of users. It’s more common in people of Asian descent with the HLA-B*58:01 gene. Testing for this gene isn’t routine in the UK, but if you develop a rash, fever, or blistering skin after starting allopurinol, stop it and see your doctor immediately.
Why does my gout keep coming back even though I’m on medication?
Two likely reasons: you’re not taking your medicine every day, or your dose isn’t high enough. Many people take allopurinol inconsistently or stop when they feel fine. Others take 100 mg daily but need 400-600 mg to reach their target uric acid level. Check your blood levels every 2-3 months until you’re stable. If your level is still above 6 mg/dL, your dose needs to go up.
Can I drink alcohol at all if I have gout?
Beer is the worst-it raises your risk by nearly 50% per daily serving. Spirits raise it by 15%. Wine? Most studies show little to no effect. If you choose to drink, limit it to 1-2 drinks per week and never binge. One 12-ounce beer a day is too much if you’re trying to prevent flares. Water, milk, and tea are far better choices.
How long does it take for tophi to disappear?
It takes time. If you keep your uric acid below 5 mg/dL for 12 months, about 70% of people see their tophi shrink or vanish completely. For larger tophi, it can take 2-3 years. The key is consistency. Stopping and starting treatment delays or prevents this process. Patience and persistence are what heal the joints.






Comments
Matthew Higgins
December 1, 2025 AT 07:35 AMBro, I thought gout was just from beer and steak. Turns out my weekend BBQs were just a slow-motion bomb ticking in my toes. I’ve had crystals sitting in my big toe for years and never knew it. Now I drink water like it’s my job. 3 liters a day, no excuses. Also, low-fat milk? I’m drinking it like it’s liquid gold now. Who knew dairy was my secret weapon?
Also, I started allopurinol last year. First month? Flare so bad I cried. Didn’t know I needed colchicine on top. Rookie mistake. Now I take it like my life depends on it-because it kinda does.
TL;DR: Gout isn’t a party foul. It’s a silent war in your joints. And you’re the general. Show up.
Scott Collard
December 2, 2025 AT 15:17 PMUric acid >6.8 mg/dL = crystal formation. NLRP3 inflammasome → IL-1β → inflammation. Classic innate immune response. Your immune system isn’t broken-it’s overzealous. But most clinicians still treat the symptom, not the mechanism. Pathetic.
jamie sigler
December 2, 2025 AT 21:36 PMSo… you’re telling me I can’t have my Sunday morning beer and eggs? And I have to take pills forever? And I can’t even stop when I feel fine? Wow. Thanks for the guilt trip, doctor.
stephen idiado
December 3, 2025 AT 23:53 PMWestern medicine fails again. Your kidneys are clogged with toxins. Fasting + black seed oil + ginger tea flushes purines. Allopurinol? Toxic. Your body doesn’t need synthetic inhibitors. It needs ancestral wisdom. Your blood pH is acidic because you eat processed carbs. Fix the root.
Subhash Singh
December 4, 2025 AT 15:14 PMThank you for this meticulously detailed exposition. I am particularly intrigued by the genetic polymorphisms in SLC2A9 and SLC22A12. Could you please elaborate on the allelic variants most commonly associated with reduced renal excretion in South Asian populations? I am curious whether the prevalence of these variants correlates with dietary patterns in India, particularly the consumption of legumes and dairy.
Additionally, I would appreciate references to any peer-reviewed studies conducted on Indian gout patients regarding urate-lowering therapy adherence rates.
Latika Gupta
December 5, 2025 AT 03:40 AMI never realized my morning soda was worse than beer. I thought diet soda was fine… but now I’m wondering if I’ve been poisoning myself for years. I’ve had two flares in the last year and thought it was just bad luck. Maybe it’s the sugar. I’m cutting it out tomorrow. I just… didn’t know.
Sullivan Lauer
December 6, 2025 AT 14:42 PMLet me tell you something real. I had gout so bad I couldn’t walk for three weeks. I thought I was done. But here’s the thing-you don’t beat gout by being strong. You beat it by being consistent. I didn’t stop taking my meds because I felt good. I didn’t skip water because I was lazy. I didn’t drink beer because I missed the taste-I missed the pain more.
My tophi used to be visible. Now? Gone. Not because I got lucky. Because I showed up every day. Even when I didn’t feel like it. Even when my doctor said ‘you’re doing great.’ I kept going. Because gout doesn’t care how you feel. It waits. And it strikes when you’re off guard.
So if you’re thinking about stopping your meds? Don’t. If you’re thinking about having that one beer? Don’t. If you’re thinking ‘I’ll start tomorrow’? Start today. Your future self will thank you. Not your future self who’s screaming in pain. Your future self who’s hiking with his grandkids. That guy? He’s still alive. And he’s not in a wheelchair.
You got this. I believe in you.
Sara Shumaker
December 6, 2025 AT 17:09 PMWhat’s wild is how much we’ve internalized gout as a ‘punishment’ for bad habits. Like it’s a moral failure. But the truth? Most people with gout didn’t choose their genes. They didn’t choose to have kidneys that hoard uric acid. And yet we shame them for eating shrimp at a wedding or drinking a glass of wine.
I think we need to reframe this. Gout isn’t about discipline. It’s about biology. It’s about a body that’s been betrayed by its own chemistry. And the real hero here isn’t the person who never had a flare-it’s the person who’s still taking their pill every morning, even when it feels pointless.
Maybe the real ‘lifestyle change’ isn’t giving up beer. Maybe it’s giving up the guilt. You’re not lazy. You’re not weak. You’re just fighting a silent war inside your joints-and you’re still showing up.
That’s not failure. That’s courage.