Kidney Clot Risk Assessment Tool
Kidney Clot Risk Assessment
This tool helps you assess your personal risk of developing kidney-related blood clots based on common risk factors. The results are for informational purposes only and should not replace professional medical advice.
Key Takeaways
- Blood clots can block blood flow in the kidneys, leading to both sudden and long‑term damage.
- Renal artery thrombosis, renal vein thrombosis, and microvascular clotting each have distinct signs and treatment paths.
- Common risk factors include hypertension, diabetes, high cholesterol, and prolonged immobility.
- Early detection through imaging and blood tests dramatically improves outcomes.
- Managing underlying conditions and, when needed, using anticoagulants can prevent clot‑related kidney injury.
When you hear the phrase "blood clot," you probably picture a deep‑vein thrombosis in the leg or a heart attack. But clots can form in the kidneys, too, and they play a surprisingly big role in many kidney problems. Below we break down how clots show up in the kidneys, why they matter, and what you can do to keep your kidneys safe.
Blood clots are semi‑solid masses of fibrin, platelets, and trapped blood cells that form when the body’s clotting system is activated. While clotting is essential to stop bleeding, an unwanted clot can block a vessel and cut off oxygen and nutrients. In the kidneys, that blockage can spark acute injury or speed up chronic decline.
Why the Kidneys Are Vulnerable
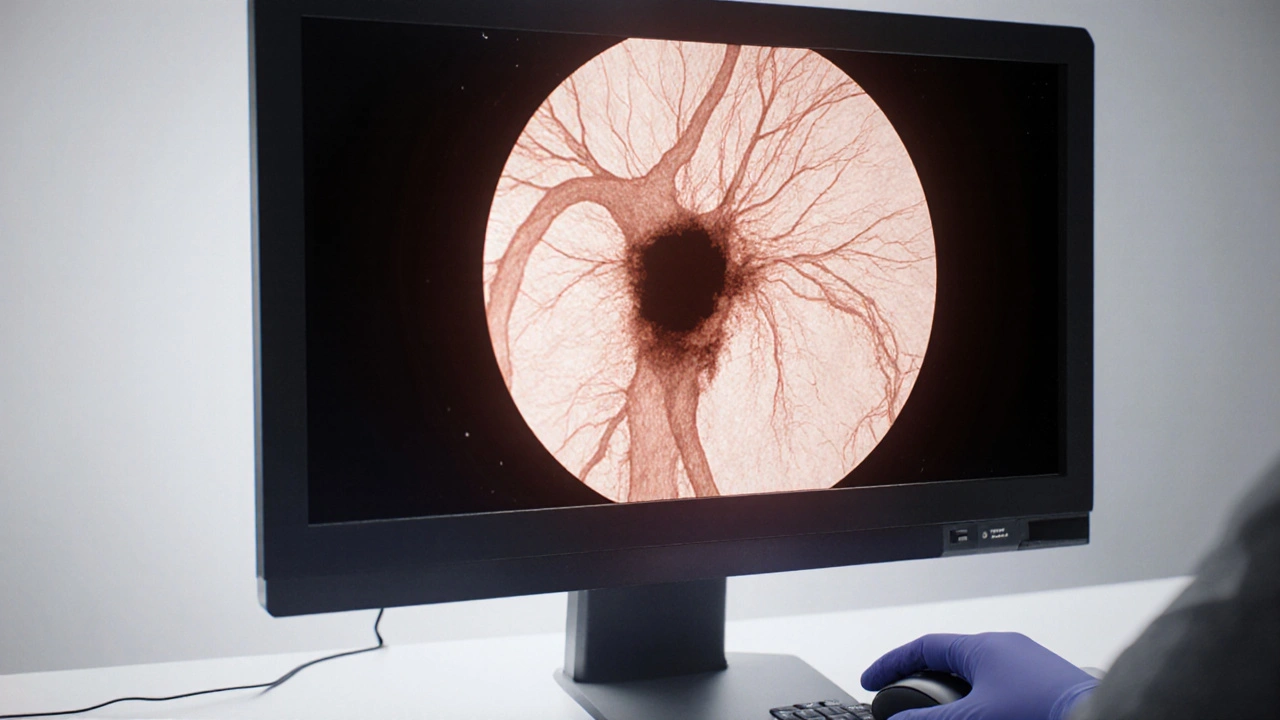
The kidneys receive about 20% of the heart’s output-roughly 1litre of blood per minute-for each kidney. That massive blood flow means any disruption can quickly affect filtration, waste removal, and fluid balance. When a clot lodges in a renal artery, vein, or the tiny capillaries that feed the glomeruli, the downstream tissue suffers from ischemia (lack of oxygen) and may scar over time.
Major Types of Kidney‑Related Clots
Three clotting scenarios dominate the conversation about kidney disease:
- Renal artery thrombosis - a clot blocks the main artery that delivers blood to the kidney.
- Renal vein thrombosis - a clot blocks the vein that carries filtered blood away from the kidney.
- Microvascular (in‑situ) thrombosis - tiny clots form inside the glomerular capillaries, often linked to systemic conditions like antiphospholipid syndrome or severe inflammation.
Each type has its own triggers, symptoms, and treatment options.
Renal Artery Thrombosis: The Sudden Shut‑Down
Renal artery thrombosis occurs when a clot fully or partially blocks the artery that supplies a kidney is a medical emergency. It often follows atrial fibrillation, severe atherosclerosis, or trauma. Because the kidney’s blood supply is cut off, patients may feel sharp flank pain, nausea, and a sudden rise in blood pressure.
Diagnosis usually involves a contrast‑enhanced CT scan or MR angiography that shows a filling defect in the renal artery. Blood tests may reveal elevated lactate dehydrogenase (LDH), a marker of tissue damage.
Treatment aims to restore flow fast. Options include systemic anticoagulation (heparin followed by warfarin or a direct oral anticoagulant), catheter‑directed thrombolysis, or, in rare cases, surgical embolectomy. Prompt therapy can salvage kidney function; delayed care often leads to irreversible loss of the affected kidney.
Renal Vein Thrombosis: The Back‑Up Traffic Jam
Renal vein thrombosis is a clot that obstructs the vein draining blood from the kidney is more common in people with nephrotic syndrome, where massive protein loss triggers a hyper‑coagulable state. Other risk factors include dehydration, malignancy, and oral contraceptive use.
Symptoms are subtler than arterial blockage: mild flank discomfort, swelling of the kidney on ultrasound, and hematuria (blood in urine). Blood work often shows low albumin and elevated clotting factors.
Imaging-usually Doppler ultrasound, CT, or MRI-confirms the clot. Management centers on anticoagulation for 3-6months, plus treatment of the underlying cause (e.g., controlling protein loss in nephrotic syndrome). In selected cases, thrombolysis or placement of a venous filter is considered.
Microvascular Thrombosis: The Silent Saboteur
Even without a big clot, tiny fibrin strands can weave through the glomeruli, narrowing the filtration slits. This microvascular thrombosis is a hallmark of conditions like:
- Antiphospholipid antibody syndrome
- Severe infections (e.g., sepsis, COVID‑19)
- Scleroderma renal crisis
- Malignancy‑associated coagulopathy
Patients may develop acute kidney injury (AKI) that rises over days, with rising creatinine, low urine output, and sometimes full‑blown hemolytic anemia. A kidney biopsy often shows “fibrin thrombi” in capillary loops.
Because the clots are microscopic, imaging rarely spots them. Treatment relies on addressing the systemic trigger and using anticoagulation or plasma exchange in severe cases. Early intervention can halt progression to chronic kidney disease (CKD).
How Common Clots Contribute to Chronic Kidney Disease
Even when clots don’t cause an acute event, repeated micro‑thrombotic injury can scar the kidney over years. Studies from 2023‑2024 estimate that up to 15% of CKD patients have a hidden hyper‑coagulable state that accelerates loss of glomerular filtration rate (GFR). Risk factors overlap heavily with those for cardiovascular disease: hypertension, diabetes, high cholesterol, and smoking.
Managing these factors reduces both heart attacks and kidney decline. For patients with documented clotting disorders, low‑dose aspirin or a direct oral anticoagulant (DOAC) may be added to the usual CKD regimen, provided bleeding risk is acceptable.
Diagnostic Toolbox: Spotting a Kidney‑Related Clot
When a clinician suspects a clot, they usually run a combination of tests:
- Imaging: CT angiography for arterial blockage; Doppler ultrasound or MR venography for venous clot; MRI for microvascular changes (rarely used).
- Blood labs: Creatinine, eGFR, LDH, D‑dimer, coagulation panel (PT/INR, aPTT), protein C & S, antiphospholipid antibodies.
- Urine analysis: Hematuria, proteinuria, and casts that hint at glomerular injury.
- Kidney biopsy (when imaging is inconclusive): Shows fibrin thrombi, ischemic changes, or inflammatory infiltrates.
Putting the pieces together lets doctors decide whether a clot is the cause, a contributor, or an incidental finding.
Treatment Landscape: From Anticoagulants to Lifestyle Tweaks
Therapy falls into two buckets: acute management (stop the clot, restore blood flow) and long‑term prevention (keep new clots from forming).
| Condition | Typical Cause | Key Symptoms | Diagnosis | Primary Treatment |
|---|---|---|---|---|
| Renal artery thrombosis | Atrial fibrillation, atherosclerosis, trauma | Sudden flank pain, nausea, hypertension | CT/MR angiography, elevated LDH | Systemic anticoagulation, catheter‑directed thrombolysis |
| Renal vein thrombosis | Nephrotic syndrome, malignancy, dehydration | Mild flank discomfort, hematuria, kidney swelling | Doppler US, CT, low albumin labs | Anticoagulation (3‑6mo), treat underlying disease |
| Microvascular thrombosis | Antiphospholipid syndrome, sepsis, scleroderma | Gradual rise in creatinine, hematuria, anemia | Kidney biopsy, coagulation panel | Targeted anticoagulation, plasma exchange, manage trigger |
For most patients, blood clots kidney disease prevention starts with controlling blood pressure, glucose, and cholesterol. Regular exercise, a balanced diet low in sodium, and staying hydrated are simple actions that keep the blood less sticky.
When a clot has already caused damage, nephrologists may add ACE inhibitors or ARBs to lower intraglomerular pressure, slowing scar formation.
Living With a History of Kidney‑Related Clots
If you’ve had a clot, follow these practical steps:
- Take any prescribed anticoagulant exactly as directed. Missing doses can let the clot grow.
- Schedule regular blood work (INR, creatinine, platelet count) to catch side effects early.
- Monitor blood pressure daily; uncontrolled hypertension is a major clot trigger.
- Watch for warning signs: sudden flank pain, new blood in urine, swelling in legs, or unexplained fatigue.
- Stay active-short walks after meals improve circulation and reduce clot risk.
- Talk to your doctor before starting new supplements or over‑the‑counter meds, especially NSAIDs which can worsen kidney function.
Most importantly, keep an open line with your healthcare team. Adjustments to medication or diet can be made quickly if lab results shift.
Frequently Asked Questions
Can a blood clot cause chronic kidney disease without an acute event?
Yes. Repeated micro‑vascular clotting can scar the glomeruli over months or years, slowly lowering the glomerular filtration rate. This process often goes unnoticed until routine labs show a steady rise in creatinine.
What are the most common risk factors for renal vein thrombosis?
Nephrotic syndrome is the leading cause, followed by malignancy, severe dehydration, and certain hormonal medications. Patients with these conditions should be assessed for hyper‑coagulability early.
Is it safe to take aspirin if I have chronic kidney disease?
Low‑dose aspirin (81mg) is often safe and can reduce clot risk, but it should only be used under a doctor’s guidance because it may increase bleeding risk, especially if you’re already on an anticoagulant.
How quickly can kidney function recover after a renal artery clot is cleared?
If blood flow is restored within hours, many patients regain most of the lost function. Delays beyond 24hours often lead to permanent loss of the affected kidney tissue.
Do lifestyle changes really lower the risk of clot‑related kidney injury?
Absolutely. Regular exercise, a Mediterranean‑style diet, staying well‑hydrated, and controlling blood pressure and diabetes have been shown in large cohort studies to cut the incidence of both cardiovascular clots and kidney‑related thrombotic events by 20‑30%.







Comments
Claire Mahony
October 15, 2025 AT 05:46 AMThere’s a lot of hype around clot‑related kidney injury, but most patients never see a major event if they keep their blood pressure in check and quit smoking.
Andrea Jacobsen
October 16, 2025 AT 09:33 AMI agree, Claire. It’s easy to get alarmed by the scary headlines, yet the practical steps-regular labs, a low‑salt diet, and staying active-make a huge difference. People often overlook how much a simple blood pressure cuff can prevent downstream clot formation. Also, staying hydrated after a long flight helps keep the circulation humming. Bottom line: consistency beats panic.
Jessica Gentle
October 17, 2025 AT 13:20 PMWhen you dig into the pathophysiology, you’ll see that the kidney’s unique microcirculation makes it a prime target for thrombotic insults. First, the organ receives roughly 20 % of cardiac output, so any clot that narrows a renal artery can cause a rapid drop in perfusion pressure. Second, the glomerular capillaries are tiny, high‑pressure filters; even micro‑thrombi can obstruct filtration and trigger a cascade of inflammation. Third, conditions like nephrotic syndrome increase circulating fibrinogen and decrease antithrombin III, creating a hyper‑coagulable milieu. Fourth, systemic diseases such as antiphospholipid syndrome or severe COVID‑19 infection can seed clots directly within the glomeruli. Fifth, the renal vein’s low‑pressure system means that a clot there can back up blood, leading to congestion, hematuria, and a rise in creatinine. Sixth, imaging advances-especially contrast‑enhanced CT angiography-allow clinicians to pinpoint arterial occlusions within minutes of symptom onset. Seventh, treatment timing is critical: re‑establishing flow within six hours of an arterial thrombus can salvage up to 80 % of renal function, whereas delays beyond 24 hours often result in irreversible loss. Eighth, anticoagulant selection now includes direct oral anticoagulants (DOACs) for many patients, offering a more convenient alternative to warfarin with fewer dietary restrictions. Ninth, lifestyle modifications remain the backbone of prevention; controlling hypertension, diabetes, and dyslipidemia reduces both cardiovascular and renal clot risk. Tenth, regular monitoring of proteinuria in diabetic patients can serve as an early warning sign of underlying microvascular injury. Eleventh, renal biopsies, while invasive, are sometimes the only way to visualize fibrin thrombi in the glomerular loops and guide therapy. Twelfth, multidisciplinary care-nephrology, hematology, and interventional radiology working together-optimizes outcomes. Thirteenth, patient education about symptoms such as sudden flank pain, new hematuria, or unexplained hypertension can prompt earlier presentation. Fourteenth, for those with a history of clotting, low‑dose aspirin or a tailored DOAC regimen may be justified, but this must be balanced against bleeding risk. Fifteenth, ongoing research into novel antithrombotic agents and biomarkers holds promise for more personalized risk stratification. In summary, while the clot‑kidney link sounds alarming, a combination of vigilant screening, prompt imaging, and aggressive management of underlying risk factors can dramatically improve prognosis.
Samson Tobias
October 18, 2025 AT 17:06 PMThat was a thorough rundown, Jessica. I’d add that patients often feel overwhelmed by the sheer number of labs, so it helps to schedule a single “kidney‑check” day where blood work, urine analysis, and possibly a Doppler are done together. Also, don’t forget to review medication lists-NSAIDs and certain supplements can tip the balance toward clot formation. Encouraging a short walk after meals can improve venous return, which is a simple but effective habit. Finally, keeping a symptom diary can make it easier for the care team to spot patterns early.
Alan Larkin
October 19, 2025 AT 20:53 PMHonestly, most of this info is already on Wikipedia.
John Chapman
October 21, 2025 AT 00:40 AMWhile Wikipedia is a handy springboard, it often glosses over the nuances that clinicians need to make evidence‑based decisions. For instance, the distinction between arterial and venous thrombi isn’t just semantic; it dictates whether you choose thrombolysis or anticoagulation, and that decision hinges on imaging findings that are rarely covered in a general article. Moreover, the latest consensus statements from the KDIGO workgroup recommend specific D‑dimer thresholds for initiating work‑up, which are absent from most lay‑person resources. So, a deeper dive into primary literature is essential for anyone managing these patients.
Tiarna Mitchell-Heath
October 22, 2025 AT 04:26 AMLook, if you’re not already on a DOAC, you’re basically asking for trouble. Stop playing it safe and get the prescription now.
Katie Jenkins
October 23, 2025 AT 08:13 AMLet’s get factual: the incidence of renal vein thrombosis in nephrotic syndrome is about 5‑10 %, not the 50 % some blogs claim. Also, the diagnostic yield of Doppler US for arterial occlusion is roughly 70 %, meaning a negative study doesn’t rule out disease. And don’t forget that contrast‑enhanced MR angiography has a sensitivity of 95 % for detecting renal artery thrombi, which is why it’s the gold standard in many centers. Lastly, the phrase “clot‑related kidney injury” is a bit of a buzzword; the underlying pathophysiology is always tied to a specific cascade-whether it’s platelet activation, coagulation factor imbalance, or endothelial dysfunction.
Maggie Hewitt
October 24, 2025 AT 12:00 PMWow, Katie, you sure love the numbers. Maybe sprinkle a little humanity into those stats?
Mike Brindisi
October 25, 2025 AT 15:46 PMactually numbers are better they dont have feelings anyway lol
Steven Waller
October 26, 2025 AT 18:33 PMOne perspective that often gets missed is how patients interpret risk. When we talk about “high‑risk” scores, many imagine an imminent catastrophe, which can lead to anxiety and even non‑adherence. Framing the discussion around controllable factors-like diet, activity, and medication adherence-helps keep the conversation constructive. It’s also useful to remind patients that risk scores are probabilistic, not deterministic, and that early interventions can shift the curve dramatically.
Puspendra Dubey
October 27, 2025 AT 22:20 PMYo bro, life’s a drama queen itself, but when the kidneys start throwing a tantrum, you gotta whisper sweet nothings and pray to the gods of blood‑flow, lol.
Shaquel Jackson
October 29, 2025 AT 02:06 AMOk, I get it, drama. But if you’re already on a blood thinner, maybe just chill and let the meds do their thing instead of going full‑on theater.