Automated Dispensing Cabinets (ADCs) are meant to make medication delivery safer in clinics and hospitals. But they don’t fix errors by themselves. In fact, when used wrong, they can make things worse. A 2017 case at a U.S. hospital showed a patient getting 10 times the right dose of insulin because the cabinet was misconfigured. That’s not rare. Studies show that in six out of seven nursing units, ADCs actually led to more than a 30% increase in dispensing errors when staff weren’t trained properly or the system wasn’t set up right.
What Exactly Is an Automated Dispensing Cabinet?
An Automated Dispensing Cabinet (ADC) is a locked, computer-controlled box that stores medications at the point of care-like on a hospital floor or in a clinic exam room. It’s not just a fancy medicine drawer. Modern systems like the BD Pyxis MedStation is a computerized medication storage system used in acute care settings with barcode scanning and EHR integration, Omnicell XT is a pharmacy automation system with temperature-controlled compartments and override tracking, or Capsa NexsysADC is a compact automated dispensing system designed for ambulatory clinics with HL7 integration do more than hold pills. They track who takes what, when, and why. They scan barcodes to match the right drug to the right patient. They lock away controlled substances like fentanyl and oxycodone. And they connect to your electronic health record so the pharmacist can see what’s being given.
But here’s the catch: if the cabinet doesn’t know who the patient is, or if the nurse can bypass safety checks too easily, the system becomes a liability. The Institute for Safe Medication Practices (ISMP) says ADCs only reduce errors when they’re part of a larger safety plan-not a magic fix.
Why Do ADCs Sometimes Cause More Errors?
It’s not the machine. It’s how we use it.
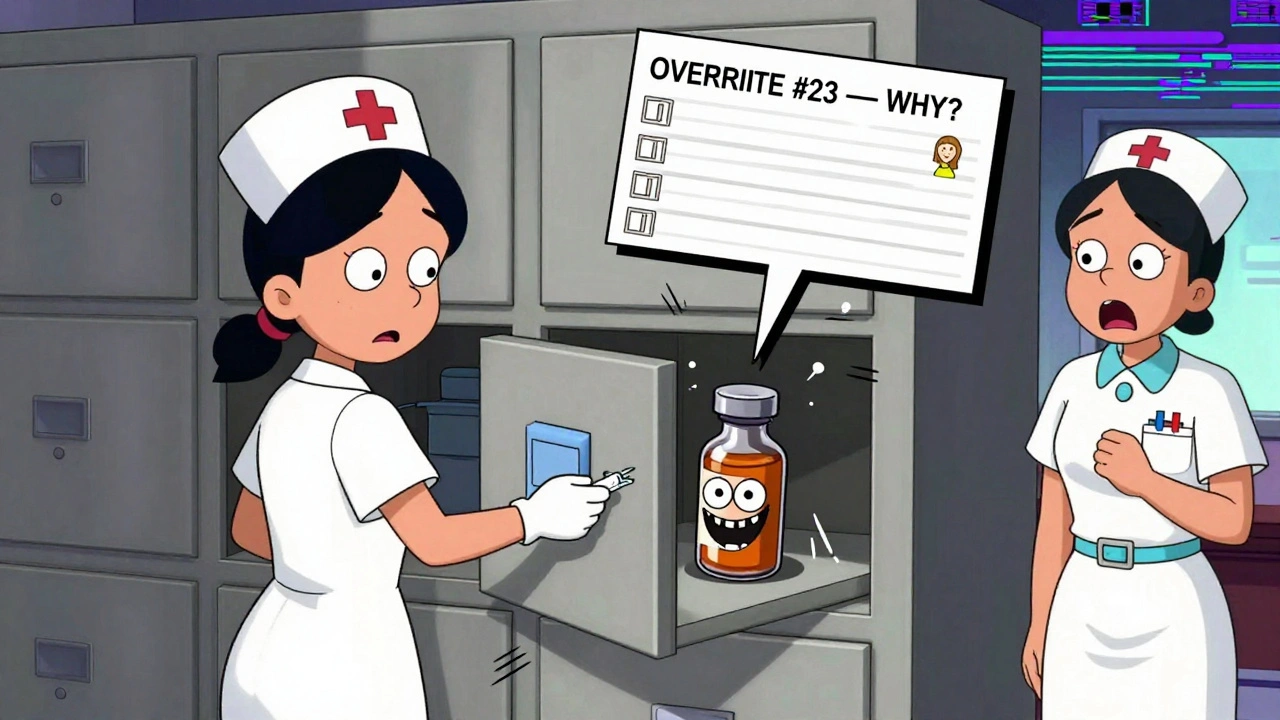
One big problem is override functions. These let staff take medication without scanning a barcode or confirming the patient’s identity. That’s useful in emergencies-like when someone’s crashing and needs epinephrine right now. But if nurses can override the system 20 times a shift without logging why, mistakes pile up. A 2021 ISMP audit found that 58% of facilities had unchecked override use. In one ICU, a nurse grabbed naloxone instead of fentanyl because both were in the same drawer, and the system didn’t block it. The nurse caught it before giving it-but only because she double-checked.
Another issue is bad layout. Look-alike, sound-alike drugs-like morphine and hydromorphone-should never be placed next to each other. But in many cabinets, they are. One study showed that when these drugs were separated and labeled clearly, wrong-medication errors dropped by 41%.
Then there’s the problem of restocking. If a pharmacy tech loads the wrong drug into a drawer because they misread the label, the cabinet won’t know. It just stores what you put in. And if the system isn’t linked to the pharmacy’s computer, there’s no pharmacist reviewing what’s being stocked. That’s a major gap. The ISMP says every ADC should require pharmacist approval before any new drug is added to the system.
How to Set Up an ADC the Right Way
Getting ADCs right starts before you even unbox them.
- Build a team. Don’t let pharmacy or nursing do this alone. Bring in IT, clinical staff, and even a patient safety officer. Everyone who uses the system should have a say in how it’s configured.
- Map your meds. List every drug you’ll store. Group them by use: pain meds, antibiotics, cardiac drugs. Then put high-risk drugs-like insulin, heparin, and opioids-in separate drawers with extra locks.
- Enforce barcode scanning. Every time a drug is taken out, the system must scan the patient’s wristband and the medication’s barcode. No exceptions. Even for "routine" meds.
- Lock down overrides. Only allow overrides for true emergencies. Require a second licensed provider to witness every override. Log the reason every time. And cap how many override doses one person can take in a shift.
- Place meds smartly. Put the most-used drugs at eye level. Keep refrigerated meds away from the cabinet’s screen or power units. Store look-alike drugs on opposite sides of the cabinet.
- Link to your EHR. The cabinet must talk to your electronic health record. That way, it can check for allergies, duplicate orders, and drug interactions before allowing a dose to be taken.
And don’t forget cleaning. During the pandemic, many clinics started keeping disinfectant wipes right next to the ADC. That’s not a luxury-it’s a must. Studies show that 40% fewer surface contaminants occur when staff wipe down the cabinet after each use.
Training Is Not Optional
You can’t just hand someone a badge and say, "Go use the Pyxis."
A 2022 survey of 850 pharmacists found that 31% said poor training was the top reason for ADC errors. Nurses need to know how to:
- Scan barcodes correctly-don’t just wave the wand near the label
- Recognize when the system is giving a warning (like "potential interaction with warfarin")
- Understand override protocols and when they’re allowed
- Report system glitches immediately
Most vendors offer training, but it’s often too short. A 2022 Omnicell report found that staff need 4 to 6 weeks to become truly competent. Set up shadowing. Do weekly drills. Test people after 30 days. Make sure they can explain why they’re doing something, not just how.
What to Watch Out For
Even with good setup and training, things go wrong. Here are the top 5 red flags:
- Overused overrides. If your unit has more than 10 overrides per day per nurse, something’s broken.
- Same drawer, different drugs. If you see insulin and glucagon side by side, fix it now.
- No pharmacist review. If the cabinet isn’t connected to the pharmacy system, you’re flying blind.
- Expired meds in the cabinet. ADCs don’t auto-remove expired drugs. Someone has to check.
- Staff avoiding the system. If nurses are grabbing meds from the crash cart instead of the ADC, ask why. Is it too slow? Too confusing? Too many steps?
A 2020 case at Johns Hopkins showed that when they reduced override use by 50% and added mandatory double-checks, medication timing errors dropped by 27%. That’s not luck. That’s design.
What’s New in 2025?
Technology is catching up. Omnicell released AI tools in early 2024 that detect unusual patterns-like a nurse taking 5 doses of morphine in 15 minutes-and flag potential diversion. BD Pyxis is rolling out biometric login (fingerprint or palm scan) in late 2025 to replace passwords, which are too easy to share.
And integration is getting smarter. By 2026, 78% of ADCs are expected to use HL7 FHIR, a modern standard that lets them pull real-time data from the EHR-like a patient’s latest kidney function test-before allowing a dose of a nephrotoxic drug.
But the biggest change isn’t tech. It’s culture. More clinics are now measuring ADC safety like they measure infection rates: daily audits, incident reports, and team huddles to review near-misses. That’s what turns a machine into a safety tool.
Final Thought: It’s Not About the Cabinet
The ADC isn’t the hero. It’s the tool. The real safety comes from the people using it, the rules they follow, and the checks they never skip.
Dr. Michael Cohen of ISMP said it best: "ADCs do not improve safety unless the cabinet’s design and use are planned with attention to patient profiling and other critical factors."
If you’re setting up an ADC, don’t just buy the box. Build the system around it. Train your team. Audit your overrides. Double-check your meds. And never assume the machine will catch your mistake.
Can nurses bypass the ADC without consequences?
No, not safely. Every override must be logged with a reason and witnessed by another licensed provider. Facilities that allow unchecked overrides see error rates 2.3 times higher than those with strict controls. Most hospitals now track override frequency monthly and investigate spikes.
Are ADCs better than manual dispensing?
Yes-when used correctly. Studies show ADCs reduce dispensing errors by 15-20% compared to manual unit-dose systems. But if the cabinet isn’t linked to the pharmacy system or staff aren’t trained, errors can increase by over 30%. The machine doesn’t fix bad processes-it amplifies them.
Do ADCs prevent all medication errors?
No. ADCs help prevent wrong drug, wrong dose, and wrong patient errors-but they can’t catch everything. They don’t stop wrong route (like giving an IV drug orally) or wrong timing. They also can’t detect if a nurse misreads a handwritten order. ADCs are one layer of safety, not the whole system.
How often should ADCs be audited?
At least monthly. Audits should check for expired medications, incorrect restocking, unexplained overrides, and mismatched barcodes. The Joint Commission expects facilities to document these audits. Some high-risk units, like ICUs, do weekly spot checks.
What’s the cost of an ADC for a small clinic?
For a small ambulatory clinic, a compact unit like Capsa’s 4T countertop model costs between $15,000 and $25,000. Larger systems like Omnicell XT can run $25,000-$45,000. But cost isn’t just the machine-it includes training, pharmacy integration, and ongoing maintenance. Budget for at least $5,000-$10,000 more in setup and support.
Can ADCs store controlled substances?
Yes, and they’re required to. All major ADCs have DEA-compliant compartments for opioids and other controlled drugs. These drawers require dual authentication-usually a badge and a PIN or biometric scan-and must track every removal. The system automatically reports to pharmacy and DEA databases.
What should I do if the ADC crashes during a shift?
Have a backup plan. Every unit should have a locked emergency cart with essential meds and a printed list of approved doses. Staff must be trained to use it. Never bypass the ADC without documenting why. After the incident, report the system failure to IT and pharmacy immediately. Most vendors offer 24/7 support-Omnicell’s average response time is under 2 hours for critical issues.
Next Steps for Clinics
If you’re using an ADC today:
- Run a safety audit this week. Check for look-alike drugs in the same drawer.
- Review your override logs from the last 30 days. Are they under 5 per nurse per shift?
- Ask your pharmacy: Is every drug added to the ADC approved by a pharmacist?
- Train one nurse to demonstrate proper scanning and override use during your next team meeting.
If you’re thinking about getting one:
- Don’t buy based on price alone. Ask vendors for a live demo with your actual drug list.
- Insist on integration with your EHR and pharmacist review before stocking.
- Ask for their compliance with the 2019 ISMP Core Safety Processes.
- Plan for at least 6 weeks of training before going live.
Safety doesn’t come from technology. It comes from attention to detail, clear rules, and people who never stop asking, "What if?"





Comments
Scott van Haastrecht
December 5, 2025 AT 13:53 PMLet’s be real - ADCs are just glorified vending machines with a compliance sticker. The moment you let nurses override without consequence, you’re asking for trouble. That 2017 insulin case? That’s not an anomaly, it’s the default setting in half the hospitals I’ve worked in. No amount of barcode scanning fixes human laziness.
Bill Wolfe
December 6, 2025 AT 05:18 AMIt’s fascinating how we’ve outsourced clinical judgment to machines while simultaneously enabling cognitive bypasses through override functions. The irony is thick enough to spread on toast. Modern healthcare has become a theater of technological theater - where the system is designed to appear safe, not to actually be safe. The ISMP’s 2019 Core Safety Processes aren’t guidelines; they’re ethical imperatives, yet institutions treat them like optional add-ons. This isn’t a failure of engineering - it’s a failure of moral imagination.
Ollie Newland
December 6, 2025 AT 22:21 PMBeen on the front lines with Pyxis for 8 years. The biggest issue isn’t the tech - it’s the restocking. Techs grabbing meds off the wrong shelf because they’re rushed, and the system just accepts it. We started requiring dual sign-off on all new med additions last year. Drop in errors? 40%. Also - never underestimate the power of a clean cabinet. Wiping it down after every use isn’t hygiene, it’s a ritual that keeps you sharp.
Rebecca Braatz
December 7, 2025 AT 17:07 PMY’all are overcomplicating this. If you train your team right, enforce the rules, and audit like your patients’ lives depend on it - the ADC becomes your best ally. We did a 30-day drill where every nurse had to demonstrate proper scanning and override logging. Guess what? Errors dropped 35%. It’s not magic. It’s accountability. Start small. Do one thing today that makes the system work for you, not against you.
Heidi Thomas
December 8, 2025 AT 18:17 PMADCs don’t fix dumb people and you know it
Alex Piddington
December 9, 2025 AT 06:04 AMWhile I appreciate the technical depth of this post, I would respectfully emphasize the importance of institutional culture in sustaining ADC safety protocols. The human factor remains the most volatile variable in any automated system. A 2023 study in the Journal of Patient Safety demonstrated that units with structured peer-review huddles experienced 62% fewer near-misses than those relying solely on system alerts. It is not merely about configuration - it is about collective vigilance.
Dematteo Lasonya
December 9, 2025 AT 06:45 AMI’ve seen ADCs save lives and nearly kill them. The difference? Training that doesn’t end after the vendor leaves. We started doing monthly mock emergencies - one nurse gets a fake code, the other has to pull meds from the ADC under pressure. We record it. We debrief. No one gets shamed. But everyone learns. That’s how you build muscle memory, not just compliance.
Jake Deeds
December 11, 2025 AT 06:21 AMYou know what’s really scary? The fact that most hospitals still don’t require pharmacists to approve every drug added to the cabinet. It’s like letting a high school intern stock the ER. The 2021 ISMP audit found 58% of facilities had unchecked overrides - and yet nothing changes. We’re not just negligent. We’re complacent. And patients are paying the price with their lives. This isn’t a system failure. It’s a moral failure.