Many people turn to St. John’s Wort because they want a natural way to manage mild depression. It’s available over the counter, labeled as a supplement, and often marketed as safe. But here’s the truth: St. John’s Wort isn’t harmless. It can make your prescription drugs stop working - sometimes dangerously so.
Imagine taking warfarin to prevent blood clots, and suddenly your INR drops from 2.5 to 1.3. That’s not a lab error. That’s St. John’s Wort. It’s not just about feeling less depressed. It’s about whether your heart medication, birth control, or transplant drug still works at all.
How St. John’s Wort Changes How Your Body Processes Medications
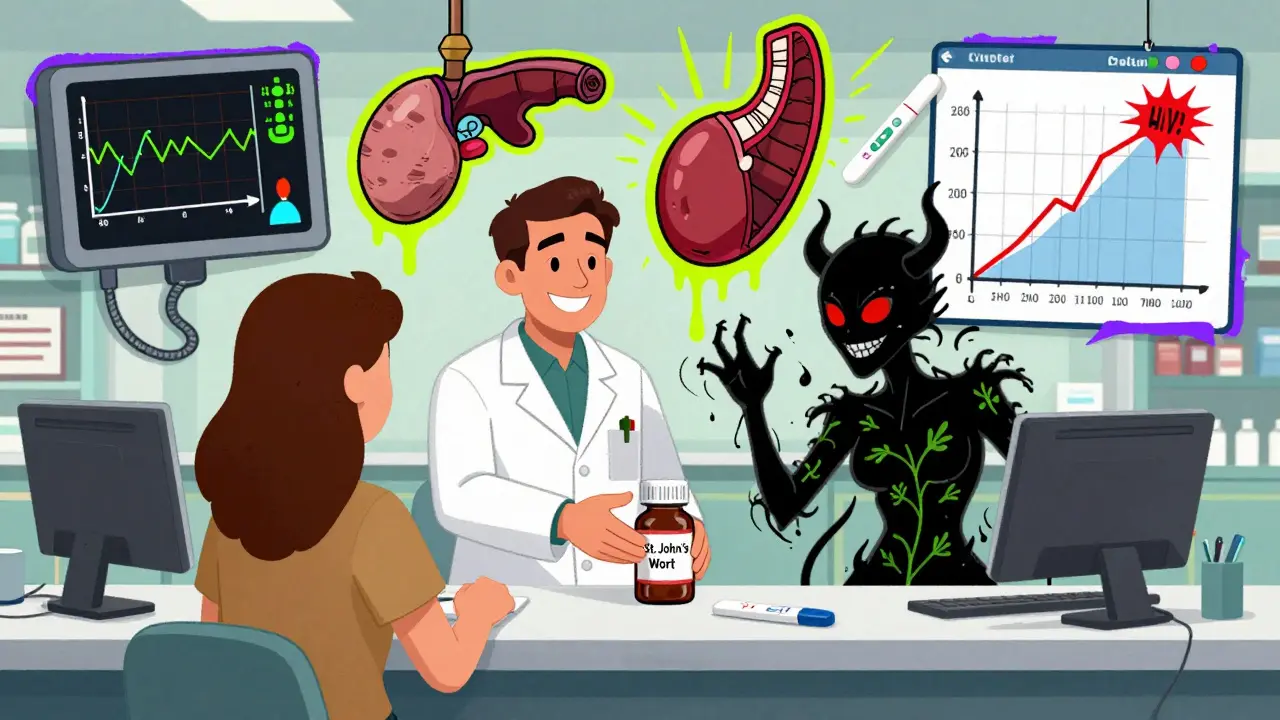
St. John’s Wort doesn’t just float through your system. It actively changes how your liver and gut handle other drugs. The key player is hyperforin - a compound in the herb that turns on enzymes like CYP3A4 and CYP2C9. These enzymes normally break down medications so your body can get rid of them. When St. John’s Wort turns them up, drugs get flushed out too fast.
Think of it like this: if your body is a factory, these enzymes are the workers who package and ship out drugs. St. John’s Wort hires extra workers, speeds up the line, and suddenly your medication doesn’t stick around long enough to work. Studies show this can reduce drug levels in your blood by 30% to 50%. That’s not a small drop. That’s the difference between a drug working and it doing nothing at all.
And it’s not just about metabolism. St. John’s Wort also affects P-glycoprotein, a protein that shuttles drugs in and out of cells. This means even drugs that aren’t broken down by liver enzymes can be pushed out of your system faster - like digoxin, used for heart failure, or cyclosporine, taken by transplant patients.
Medications That Can Become Ineffective - Or Dangerous
St. John’s Wort doesn’t pick and choose. It interferes with a long list of critical drugs. Here’s what you need to watch out for:
- Anticoagulants (warfarin, phenprocoumon): A drop in INR from 2.8 to 1.5 within 10 days has been documented. That means your blood clots faster. One case led to a stroke.
- Immunosuppressants (cyclosporine, tacrolimus): Transplant patients have seen cyclosporine levels drop by 40%. That’s not a glitch - it’s organ rejection waiting to happen.
- HIV medications (protease inhibitors, NNRTIs): Saquinavir and efavirenz levels can fall by half. That increases the risk of drug-resistant HIV.
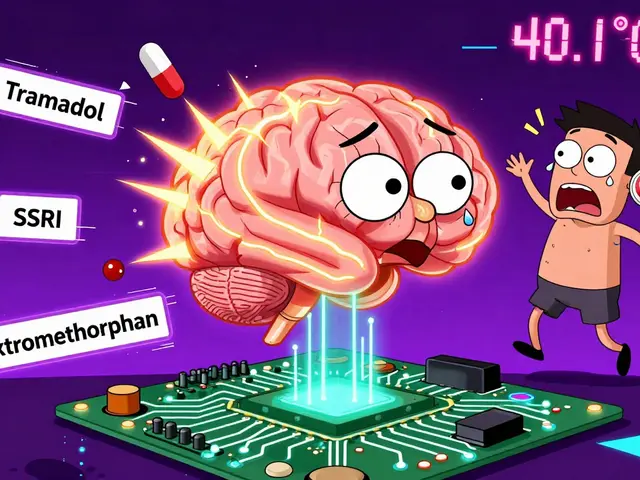
- Antidepressants (SSRIs, SNRIs, nefazodone): Combining St. John’s Wort with fluoxetine or sertraline can trigger serotonin syndrome - a life-threatening condition with high fever, confusion, and muscle rigidity. Six cases were reported in Australia alone.
- Birth control pills: Ethinyl estradiol levels drop 25-35%. There are documented cases of unintended pregnancy despite perfect pill use.
- Anticonvulsants (phenytoin, carbamazepine): Seizure control can fail. One patient had a breakthrough seizure after starting St. John’s Wort.
- Benzodiazepines (alprazolam, diazepam): Anxiety meds lose potency. Patients report sudden return of panic attacks.
- Statins (atorvastatin, simvastatin): Cholesterol control drops. Pravastatin and fluvastatin are safer - but only because they’re not metabolized the same way.
- Theophylline, digoxin, opioids, PPIs: All affected. The list goes on.
Some people think, “I’m only taking a little.” But even 300 mg a day can trigger interactions. The effect builds over days and lasts for weeks after you stop. One study found enzyme induction still active two weeks after stopping St. John’s Wort.
Why People Don’t Realize the Risk - And Why That’s Dangerous
Most users don’t tell their doctors they’re taking it. In a Johns Hopkins study of 250 people on prescription meds, 41% didn’t mention St. John’s Wort - even when asked about “other medications.” Why? Because they don’t think of it as medicine.
“It’s natural,” they say. “It’s just a herb.” But natural doesn’t mean safe. Aspirin comes from willow bark. Digitalis from foxglove. Both are deadly if misused. St. John’s Wort is no different.
Online reviews are full of success stories - “My mood lifted in 3 weeks!” - but silent on the risks. One Reddit user shared how their warfarin dose had to be increased by 25% after starting St. John’s Wort. Another reported pregnancy despite perfect birth control use. These aren’t rare. They’re predictable.
And here’s the kicker: pharmacists and doctors aren’t always asking the right question. If you ask, “Are you taking any other meds?” people say no. But if you ask, “Do you take any herbal supplements, vitamins, or over-the-counter products?” - suddenly the truth comes out.
What to Do If You’re Taking St. John’s Wort
If you’re on any prescription drug and you’re taking St. John’s Wort - stop. Don’t just cut back. Stop. Then talk to your doctor.
Don’t quit cold turkey if you’re using it for depression. Work with your provider to switch safely. Abruptly stopping St. John’s Wort can cause withdrawal symptoms like dizziness, anxiety, and irritability.
Here’s what you need to do:
- Make a full list of everything you take - including supplements, teas, and vitamins.
- Bring it to your doctor or pharmacist. Don’t assume they’ll ask.
- If you’re on warfarin, get an INR check 3-5 days after stopping St. John’s Wort.
- If you’re on cyclosporine, digoxin, or HIV meds, ask for a blood level test.
- Wait at least two weeks after stopping St. John’s Wort before starting a new medication that’s known to interact.
There’s no safe middle ground. No “low dose” that won’t interfere. The science is clear: if you’re on a prescription drug, St. John’s Wort is not an option.
What’s Changing - And What It Means for You
Regulators are catching up. The FDA now requires warning labels on St. John’s Wort products: “Ask a doctor before use if you are taking prescription drugs.” Australia has mandated interaction warnings since 2018. Germany and Sweden require prescriptions.
But the biggest shift is clinical. The American Psychiatric Association’s 2023 guidelines no longer say “St. John’s Wort may be considered” for depression. They now say: “Not recommended for patients taking any prescription medications.” That’s a huge change - based on years of documented harm.
Some researchers are exploring low-hyperforin extracts that might reduce interactions. But right now, no standardized product is proven safe with prescription drugs. The European Food Safety Authority says: “No safe threshold can be established.”
St. John’s Wort isn’t a miracle herb. It’s a powerful biochemical agent with a narrow margin of safety. And for most people on prescription meds, the risks far outweigh any potential benefit.

Alternatives That Actually Work - Without the Risk
If you’re looking for help with mild depression, there are safer, evidence-backed options:
- Cognitive Behavioral Therapy (CBT): Proven effective, no side effects, covered by most insurance.
- Exercise: Just 30 minutes of brisk walking five days a week can be as effective as antidepressants for mild depression.
- Omega-3s (EPA-rich): Studies show 1,000-2,000 mg of EPA daily can improve mood without interacting with meds.
- Vitamin D: Low levels are linked to depression. Testing and correcting deficiency is simple and safe.
- Prescription options: SSRIs like sertraline or escitalopram have decades of safety data and are well-tolerated.
None of these require you to gamble with your other medications. None of them carry a 30-50% chance of making your heart, transplant, or HIV drugs stop working.
Final Thought: Natural Isn’t Safe - And Silence Can Be Deadly
St. John’s Wort isn’t the villain. It’s just a plant. The real problem is the myth that natural = harmless. Millions of people take it without knowing it’s a drug interaction waiting to happen. And when things go wrong - a stroke, a rejected organ, an unplanned pregnancy - it’s too late.
If you’re on any prescription medication, don’t take St. John’s Wort. Not even for a week. Not even if your friend says it helped. Not even if the label says “natural.”
Your health isn’t a gamble. And your meds aren’t optional.
Can I take St. John’s Wort with my antidepressant?
No. Combining St. John’s Wort with SSRIs, SNRIs, or other antidepressants can cause serotonin syndrome - a potentially fatal condition. Symptoms include high fever, rapid heart rate, confusion, muscle twitching, and seizures. Six documented cases in Australia involved this exact combination. Even if you feel fine, the risk is real and avoidable.
How long after stopping St. John’s Wort do interactions last?
Enzyme induction from St. John’s Wort can persist for up to two weeks after you stop taking it. That means your body is still breaking down other medications faster during this time. If you’re switching to a new drug, wait at least 14 days after stopping St. John’s Wort before starting it - and check with your doctor.
Is St. John’s Wort safe if I’m not on any medications?
For someone not taking any prescription drugs, St. John’s Wort may be used cautiously for mild depression. But even then, side effects like increased sun sensitivity, dry mouth, dizziness, and gastrointestinal upset are common. It’s not risk-free. And if you start any new medication later - even an antibiotic or painkiller - you could trigger an interaction.
Do all St. John’s Wort products have the same risk?
Yes. All commercially available products contain hyperforin, the compound that triggers enzyme induction. Even products labeled “standardized” or “low hyperforin” are not proven safe with medications. The European Food Safety Authority states no safe threshold exists for users on prescription drugs. There’s no reliable way to predict how your body will respond.
Why don’t more people know about these interactions?
Because supplements aren’t regulated like drugs. Manufacturers don’t have to prove safety or interactions before selling. Many consumers assume “natural” means safe. And doctors often don’t ask about herbal supplements unless they specifically inquire. A 2022 study found 73% of patients experiencing interactions didn’t know they were at risk.






Comments
Jody Kennedy
December 26, 2025 AT 11:18 AMOkay but like… I took this stuff for 3 months last year and my anxiety just vanished. No more panic attacks. Now I’m on sertraline and I’m scared to even breathe near the supplement aisle. Why does everything have to be so damn complicated?
david jackson
December 28, 2025 AT 05:44 AMLet me tell you something that nobody talks about - St. John’s Wort doesn’t just interfere with your meds, it rewires your brain’s expectation of what ‘natural healing’ even means. You start taking it because you’re tired of Big Pharma’s price tags and side effects, but then you realize you’ve been playing Russian roulette with your liver enzymes. Hyperforin isn’t some cute little herb fairy - it’s a molecular saboteur. Studies show it induces CYP3A4 like a factory foreman on espresso, and suddenly your warfarin’s out the door before it even gets to work. I’ve seen patients on transplant meds crash their levels because they thought ‘it’s just a tea.’ One guy got rejected kidneys because he didn’t tell his doctor he was sipping ‘mood booster’ from the vitamin shop. Natural doesn’t mean gentle. It means unregulated. And unregulated means someone’s got to pay the price - and it’s usually you.
Jeanette Jeffrey
December 29, 2025 AT 13:32 PMWow. So you’re saying people are dumb for trusting herbs? Congrats, you just discovered that not everything in nature is safe. My cat eats grass and pukes. That doesn’t make grass a drug. But hey, maybe you’re right - let’s lock up every plant that’s ever had a medicinal use. Next you’ll ban aspirin because willow bark is ‘natural.’
Ellie Stretshberry
December 31, 2025 AT 13:01 PMi just started taking this last month and i didnt even know it could mess with my bp med… i feel so stupid now. my doctor never asked. i just thought it was like gummy vitamins. my bad. 😅
Dan Alatepe
January 2, 2026 AT 10:26 AMBro… I took this for my ‘existential blues’ after my dog died. Felt like a spiritual reset. Then my dad had a stroke. Turns out I was on lisinopril. Now I’m the guy who almost killed his pops with a ‘natural mood booster.’ I’m not mad. I’m just… devastated. 🙏
wendy parrales fong
January 4, 2026 AT 07:54 AMI get why people take it. We all want something simple. Something gentle. Something that doesn’t feel like a chemical assault. But the truth is, our bodies don’t care if something’s labeled ‘herbal’ or ‘pharmaceutical.’ They just react. And if you’re on meds, your body’s already dancing on a tightrope. Adding this? It’s like handing someone a chainsaw while they’re balancing. Maybe the answer isn’t banning it - but teaching people to ask before they assume. I wish my mom had known. She took it with her thyroid med for years. No one ever asked.
Angela Spagnolo
January 4, 2026 AT 21:15 PM...I just stopped taking it yesterday... I didn't realize... I'm on birth control... and I've been taking it for 8 months... I'm terrified... I think I need to go to the clinic... I'm so sorry I didn't read more... I just trusted the label... 😔
Shreyash Gupta
January 5, 2026 AT 17:29 PMlol u all scared of a plant? 🤡 I’m from India, we’ve used this for 2000 years. My grandma took it with her diabetes meds. She’s 94. Still walks 5k steps. You westerners think ‘natural’ = ‘safe’? Nah. You think ‘science’ = ‘perfect’? Also nah. Maybe your meds are the problem, not the herb. 🌿
Zina Constantin
January 6, 2026 AT 00:12 AMAs someone who moved from Nigeria to the U.S. and saw both healthcare systems - this is the exact reason I stopped trusting ‘over-the-counter’ labels here. In Lagos, if you buy something that looks like medicine, you ask a pharmacist. Here? You grab it next to the gum. I’m so glad this post exists. My cousin almost lost her kidney transplant because she thought ‘it’s just a supplement.’ Please - if you’re on meds, treat every herb like a prescription. Even if it smells like sunshine.