Opioid-Antidepressant Interaction Checker
Check Your Medication Risk
This tool identifies dangerous combinations of opioids and antidepressants that may cause serotonin syndrome.
Please select medications to check risk
Select both opioid and antidepressant to see results
Important Information
Serotonin syndrome can be life-threatening. This tool provides general guidance only. Always consult your doctor before changing medications.
It’s not just about pain relief. When you take an opioid for back pain or after surgery, you might not realize you’re also mixing chemicals that can push your brain into overdrive-sometimes with deadly results. Serotonin syndrome isn’t rare. It’s underdiagnosed, misunderstood, and often blamed on antidepressants alone. But the real danger? Opioids.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome happens when too much serotonin builds up in your nervous system. It’s not an allergy. It’s not an overdose in the traditional sense. It’s a toxic overload of a chemical your brain uses to regulate mood, movement, and body temperature. Think of it like a circuit breaker tripping because too many devices are plugged in at once. The signs come fast: confusion, shivering, muscle rigidity, high fever, rapid heartbeat, and sometimes seizures. In severe cases, it can kill within hours. The Hunter Serotonin Toxicity Criteria is what doctors use to diagnose it: if you’re taking a serotonergic drug and have one of these three things-spontaneous clonus, inducible clonus with agitation or diaphoresis, or tremor with hyperreflexia-you’re likely in serotonin syndrome. It’s not just antidepressants causing this. Opioids, especially certain ones, are quietly becoming one of the top triggers.Not All Opioids Are the Same
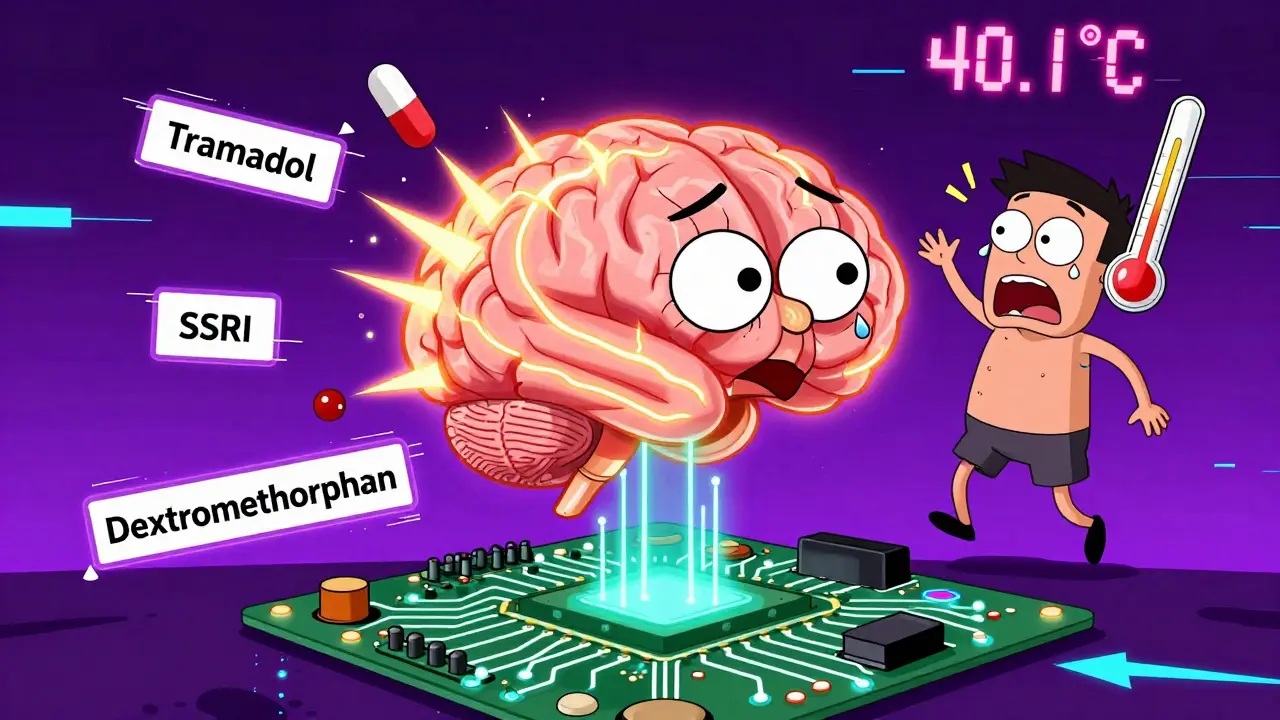
Here’s the truth most people don’t hear: opioids aren’t all created equal when it comes to serotonin. Some barely touch it. Others are practically serotonin grenades. Tramadol is the biggest red flag. It doesn’t just relieve pain-it blocks serotonin reuptake, like an SSRI. When you add it to an antidepressant like sertraline or venlafaxine, you’re stacking two serotonin boosters on top of each other. A 2021 case report described a 42-year-old woman who developed a 40.1°C fever and muscle rigidity after starting tramadol while on venlafaxine. She ended up in the ICU. Tramadol is responsible for nearly half of all opioid-related serotonin syndrome cases. Meperidine (pethidine) and dextromethorphan (yes, the cough syrup ingredient) are just as dangerous. Dextromethorphan is in dozens of over-the-counter cold medicines. People don’t think of it as a drug-until they’re taking it with fluoxetine and start sweating, shaking, and losing track of time. A 2020 review found 14 cases of serotonin syndrome from dextromethorphan and SSRIs, including three deaths-all from doses as low as 30mg a day. Then there’s fentanyl and methadone. They don’t block serotonin reuptake like tramadol, but they still bind to serotonin receptors in the brain. Fentanyl, especially at high doses used in surgery, can trigger serotonin syndrome. Methadone’s risk is lower than tramadol but still real-especially if you’re also on an SSRI that slows its metabolism. And here’s the surprise: morphine, oxycodone, and hydromorphone? They barely affect serotonin. Studies show they don’t inhibit serotonin transporters in lab tests. Yet, many doctors still avoid them out of fear. That’s unnecessary. If you’re on an antidepressant and need pain relief, these are your safest bets.The Real Culprits: Drug Combinations
The problem isn’t one drug. It’s the combo. SSRIs like fluoxetine, SNRIs like duloxetine, and even older tricyclics like amitriptyline are common. But they’re not the only ones. Triptans for migraines, certain anti-nausea drugs like ondansetron, even herbal supplements like St. John’s wort can add fuel to the fire. The real danger zone? Tramadol + SSRI. This pairing makes up 78% of all reported serotonergic drug interactions in clinical practice. The Australian Prescriber says it plainly: avoid this combo entirely. The FDA added a Black Box Warning to tramadol in January 2023 because of it. Even codeine-a drug many assume is safe-has caused serotonin syndrome in rare cases, especially when combined with other serotonergic drugs. One case involved codeine, venlafaxine, and a migraine medication. That’s three different serotonin-affecting drugs. One patient didn’t survive. And here’s the hidden risk: your body’s ability to break down these drugs matters. If you’re a poor metabolizer of CYP2D6 (a liver enzyme), tramadol won’t turn into its active painkiller form. Instead, it builds up-and so does its serotonin-blocking effect. Fluoxetine and paroxetine block this enzyme too, making the problem worse.
What Should You Do?
If you’re on an antidepressant and your doctor suggests an opioid for pain, ask these questions:- Is this opioid known to affect serotonin?
- Is there a safer alternative?
- Have you checked for interactions with my current meds?
What If You Think You Have Serotonin Syndrome?
Don’t wait. Don’t assume it’s just the flu or anxiety. If you’re on a serotonergic drug and suddenly feel:- Confused or agitated
- Shivering or sweating uncontrollably
- Muscles stiff or twitching
- Heart racing or temperature above 38°C




Comments
Jose Mecanico
January 12, 2026 AT 03:19 AMHad a friend go through this last year after mixing tramadol with sertraline. Didn’t even know it was a thing until he was in the ER. Scary stuff. Glad someone’s putting this out there.
Always assumed opioids were just for pain. Never realized some of them are basically antidepressants in disguise.
Alex Fortwengler
January 13, 2026 AT 05:57 AMOf course the FDA only acts after people die. They knew about this for decades. Big Pharma doesn’t want you to know that your cheap painkiller is a serotonin bomb. They’d rather you die quietly than lose profits on brand-name SSRIs.
And don’t get me started on how dextromethorphan is sold like candy. Next they’ll say aspirin causes brain rot.
jordan shiyangeni
January 15, 2026 AT 03:15 AMIt is profoundly irresponsible that the medical establishment continues to normalize polypharmacy without adequate pharmacokinetic education for either prescribers or patients. The biochemical interplay between serotonin reuptake inhibition and mu-opioid receptor agonism is not merely theoretical-it is empirically documented in peer-reviewed toxicology journals since at least 2003.
Furthermore, the conflation of pharmacodynamic risk with pharmacogenetic vulnerability is a critical oversight. Individuals who are CYP2D6 poor metabolizers are not simply ‘at risk’-they are biologically predisposed to lethal serotonin accumulation when exposed to tramadol, particularly when co-administered with fluoxetine, which is itself a potent CYP2D6 inhibitor. This is not a coincidence. It is a biochemical inevitability.
And yet, pharmacists still dispense these combinations without warning. That is not negligence. That is malpractice. The fact that this has become systemic speaks to the complete collapse of clinical pharmacology standards in primary care.
It is also worth noting that the Hunter Criteria, while useful, are not universally applied. Many ERs still misdiagnose serotonin syndrome as neuroleptic malignant syndrome or heat stroke. This diagnostic confusion leads to delayed treatment, increased morbidity, and unnecessary mortality.
There is no excuse for this. We have the tools. We have the data. We have the guidelines. What we lack is the will to enforce them.
Abner San Diego
January 16, 2026 AT 12:00 PMWhy are we even talking about this? If you’re on antidepressants, don’t take random pills. Simple. If you’re in pain, go to a real doctor-not some online clinic that pushes tramadol like it’s Advil.
And stop blaming Big Pharma. People are dumb. They take cough syrup with their Zoloft because they think it’s ‘natural.’ You can’t fix stupid.
Also, morphine? Yeah, safe. But good luck getting that without a police background check these days. Meanwhile, dextromethorphan’s on every shelf. That’s the real problem.
Eileen Reilly
January 17, 2026 AT 00:07 AMOMG I JUST REALIZED I TOOK DEXTROMETHORPHAN LAST WEEK WITH MY SSRIS 😭😭😭 AM I GONNA DIE??
Also why is tramadol even a thing?? Like who thought this was a good idea??
Also my pharmacist never said anything. I’m so mad rn.
Audu ikhlas
January 18, 2026 AT 04:10 AMThis is what happens when Africans and Asians are not in charge of medicine. In my country, we know opioids are for pain, not mood. We don’t mix them with antidepressants because we respect the science.
But here? Everyone’s on something. You take two pills, then three, then a cough syrup, then a herbal tea, then you wake up shaking in a hospital.
It’s not the drugs. It’s the people. Too many pills, too little discipline.
Sonal Guha
January 18, 2026 AT 18:13 PMTramadol is the real villain here not the SSRIs. OTC dextromethorphan is a ticking time bomb. Morphine is the only safe opioid if you’re on antidepressants. Period.
TiM Vince
January 18, 2026 AT 23:34 PMI’m from the Philippines. Here, tramadol is sold over the counter like candy. No prescription. No warning. People take it for headaches, for anxiety, for sleep. I’ve seen friends end up in the hospital. No one knows why.
Doctors here don’t even know what serotonin syndrome is. They think it’s ‘nervous breakdown.’
It’s not just an American problem. It’s a global blind spot. We need education, not just warnings.
And yes-dextromethorphan in cough syrup? That’s the quiet killer. No one thinks it’s a drug until it’s too late.
Thank you for writing this. Someone needed to say it out loud.