When you pick up a generic pill at the pharmacy, you might wonder: is this really the same as the brand-name drug? The answer isn’t just yes - it’s rigorously proven. The FDA doesn’t just approve generic drugs because they’re cheaper. They approve them because they’ve passed a battery of tests that prove they work the same way, in the same amount of time, with the same safety profile. This isn’t guesswork. It’s science, enforced by strict rules that every generic manufacturer must follow - no exceptions.
What Makes a Generic Drug ‘Equivalent’?
The FDA defines two key types of equivalence: pharmaceutical and bioequivalence. Pharmaceutical equivalence means the generic has the same active ingredient, strength, dosage form (like tablet, capsule, or injection), and route of administration (oral, topical, etc.) as the brand-name drug. It also must be used for the same medical conditions. That’s the baseline.
But here’s where most people get confused: two pills can have the same active ingredient and still behave differently in your body. That’s why bioequivalence matters more. The FDA requires that the generic drug delivers the active ingredient into your bloodstream at the same rate and to the same extent as the brand-name version. This isn’t about appearance - your generic might be a different color or shape. It’s about what happens inside you.
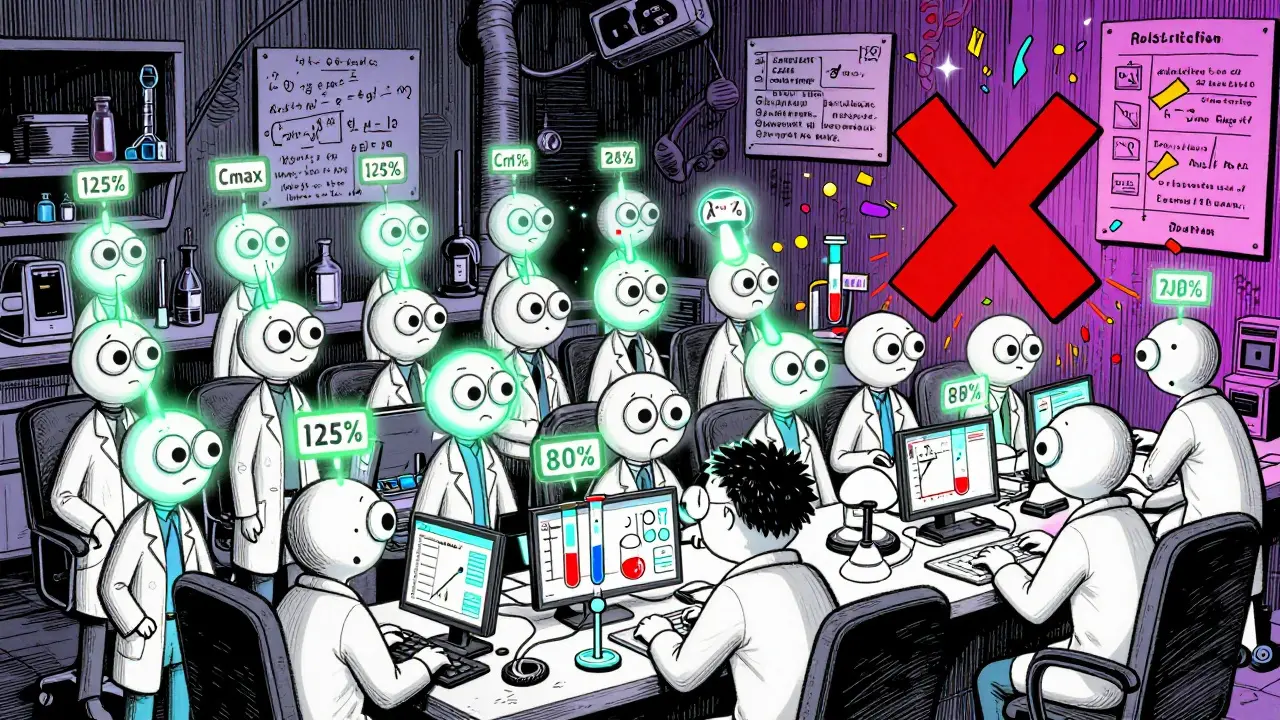
To prove this, manufacturers run bioequivalence studies using 24 to 36 healthy volunteers. Blood samples are taken over time to measure two critical numbers: Cmax (the highest concentration in the blood) and AUC (how much of the drug is absorbed overall). The FDA demands that the 90% confidence interval for both values falls between 80% and 125% of the brand-name drug’s results. If it doesn’t, the application gets rejected. No exceptions. No shortcuts.
How the FDA Tests Generic Drugs
Bioequivalence studies are just one part of the puzzle. Before a generic drug even reaches volunteers, it goes through a long chain of lab and manufacturing checks. Every batch must pass identity, strength, purity, and quality tests using validated methods. These aren’t simple spot checks - they’re full analytical profiles that compare the generic to the original brand drug down to the molecular level.
For simple pills, this might mean testing dissolution rates - how quickly the drug breaks down in simulated stomach fluid. For complex products like inhalers, topical creams, or long-acting injectables, the testing gets much more detailed. The FDA has issued over 2,100 product-specific guidances for these harder-to-copy drugs. These guidances require manufacturers to prove ‘Q3 sameness’ - meaning the generic matches the reference drug in structure, particle size, rheology, and even how it sticks to skin or lung tissue. Some of these tests didn’t even exist 15 years ago. The science has evolved, and so have the rules.
Stability testing is another non-negotiable. Generics must show they stay effective and safe over their entire shelf life. That means storing samples at 40°C and 75% humidity for six months (accelerated conditions) and at normal room temperature for 12 to 24 months (real-world conditions). If the drug degrades too fast or forms impurities, it’s rejected. No matter how cheap the production cost.
Manufacturing Standards: cGMP Applies to Everyone
It doesn’t matter if you’re a startup or a Fortune 500 company - if you make generic drugs in the U.S., you follow the same rules as Pfizer or Merck. These are the Current Good Manufacturing Practices, or cGMP, written into federal law (21 CFR Parts 210 and 211). The rules cover everything: how raw materials are received and stored, how equipment is cleaned, how production lines are monitored, and how finished products are tested before release.
Every step must be documented. Every change must be reviewed. Every batch must be traceable. The FDA doesn’t just review paperwork - they show up unannounced. In 2023, they conducted around 3,500 inspections of manufacturing sites worldwide. About half of all generic drugs in the U.S. are actually made by the same companies that make the brand-name versions - often in the same factories. That’s not a loophole. It’s by design. The FDA knows that if a facility can make a brand-name drug to exacting standards, it can make the generic too.
The ANDA Process: How Long Does Approval Take?
Getting a generic drug approved isn’t quick. It starts with an Abbreviated New Drug Application (ANDA). Unlike brand-name drugs, which need full clinical trials, generics rely on the safety data already proven by the original drug. But that doesn’t mean less work - it means smarter work. The ANDA must include detailed chemistry, manufacturing, and control data. It must prove bioequivalence. It must show stability. It must prove the facility meets cGMP.
Under the Generic Drug User Fee Amendments (GDUFA), the FDA has committed to reviewing standard ANDAs within 10 months. That’s a big improvement from the 3- to 5-year wait times before 2012. In 2022 alone, the FDA approved 892 original ANDAs and issued 478 complete response letters - meaning the application was rejected or needed major fixes. The approval rate is high, but the bar is higher.
For complex generics - like those with multiple active ingredients or unusual delivery systems - the process can take longer. The FDA now offers a Pre-ANDA program, where manufacturers can meet with regulators early to clarify testing requirements. In 2022, over 1,200 of these meetings took place. This isn’t favoritism - it’s efficiency. It prevents costly rejections down the line.
Why Do Some People Say Generics Don’t Work the Same?
Most people don’t notice a difference. A 2022 Consumer Reports survey found 89% of users were satisfied with generics, and 62% chose them specifically to save money. On Reddit’s r/pharmacy, 83% of 1,427 respondents reported no difference between brand and generic versions.
But there are exceptions. A 2021 study in JAMA Internal Medicine found that 12.3% of patients taking levothyroxine (a thyroid medication) had noticeable changes in their thyroid levels after switching between different generic brands. That’s because levothyroxine has a narrow therapeutic index - tiny differences in absorption can cause real effects. For drugs like this, the FDA recommends staying on the same generic brand unless directed otherwise by a doctor.
Similarly, some epilepsy patients report seizure breakthroughs after switching generics. While large studies haven’t confirmed a systemic problem, the FDA acknowledges that for certain high-risk drugs, even small variations in inactive ingredients or dissolution rates can matter. That’s why they’ve invested $15.7 million since 2023 into developing better testing methods for these complex cases.
It’s not that generics are unsafe. It’s that a few drugs need extra care. The FDA doesn’t treat all generics the same. They tailor the rules to the risk.

How Much Do Generics Really Save?
More than $37 billion in 2022 alone. That’s the number the FDA cites. Generics make up over 90% of all prescriptions filled in the U.S., but they account for only about 23% of total drug spending. That’s the power of competition. Before generics, a single brand-name drug could cost $500 a month. Now, the same active ingredient might cost $10. And it’s not just about price - it’s about access. Millions of people who couldn’t afford their medication now take it because generics exist.
The market is growing fast. In 2022, the U.S. generic drug market was worth $135.7 billion. By 2027, it’s projected to hit $180.3 billion. That growth isn’t just from more pills - it’s from better science. More complex drugs are going generic. More patients are trusting them. More doctors are prescribing them.
What You Can Trust
When you see ‘FDA-approved generic’ on your prescription bottle, you’re seeing a stamp of scientific rigor. The FDA doesn’t approve drugs based on cost. They approve them based on data - thousands of data points, hundreds of tests, dozens of inspections. The system isn’t perfect, but it’s transparent, science-driven, and constantly improving.
For 99% of medications, generics are not just safe - they’re identical. For the few that require extra caution, the FDA has built in safeguards. You don’t need to fear generics. You need to understand them. And when you do, you’re not just saving money - you’re using a system designed to protect your health, not just your wallet.
Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to prove they deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. This is called bioequivalence, and it’s tested in clinical studies with healthy volunteers. Over 90% of prescriptions filled in the U.S. are generics, and studies show they work just as well for most conditions.
Why do generic pills look different from brand-name ones?
The law allows differences in color, shape, size, and inactive ingredients (like fillers or coatings) because these don’t affect how the drug works. Only the active ingredient must match. These differences exist because manufacturers can’t copy the brand’s trademarked appearance, but the medicine inside is identical.
Do generic drugs have the same side effects?
Yes. Since the active ingredient and how it’s absorbed are the same, the side effect profile is identical. Any differences in side effects reported by patients are usually due to variations in inactive ingredients, which can rarely cause minor reactions like stomach upset or allergic responses - but these are uncommon and not related to the drug’s effectiveness.
Can I switch between different generic brands?
For most drugs, yes. But for medications with a narrow therapeutic index - like levothyroxine, warfarin, or certain seizure drugs - switching between generics can sometimes cause small changes in blood levels. If you’re on one of these, talk to your doctor before switching. Many pharmacies will keep you on the same generic brand unless you or your doctor requests a change.
Are generic drugs made in the same factories as brand-name drugs?
Yes - about half of all generic drugs in the U.S. are made by the same companies that produce the brand-name versions, often in the same facilities. The FDA inspects all these sites equally, whether they’re making a $500 brand drug or a $5 generic. Quality standards don’t change based on price.
How does the FDA ensure quality in overseas factories?
The FDA inspects over 3,500 manufacturing sites globally each year, including facilities in India, China, and other countries. They use the same cGMP standards as U.S. plants. If a site fails inspection, the FDA can block imports until problems are fixed. In 2022, they issued warning letters to 127 foreign facilities and halted imports from 23 of them.





Comments
Robin Keith
January 29, 2026 AT 12:16 PMLook, I get it-people think generics are just knockoffs, like a Walmart version of a Gucci bag-but that’s not how pharmacology works. The FDA doesn’t care if your pill is blue or round or smells like mint; they care about the molecular dance happening in your bloodstream. Cmax, AUC, 80–125% confidence interval-these aren’t buzzwords, they’re the bedrock. I’ve read the guidances. I’ve seen the stability reports. The science isn’t sexy, but it’s bulletproof. And yet, somehow, we still live in a world where someone will pay $200 for a brand-name antidepressant because they ‘feel’ better, even though their blood levels say otherwise. It’s not placebo-it’s narrative. And we’re all addicted to the story.