When you’re pregnant, every pill, supplement, or over-the-counter medicine feels like a high-stakes decision. You want to feel better - whether it’s heartburn, nausea, or high blood pressure - but you also don’t want to risk your baby’s health. That’s why so many expectant mothers ask: Are generic medications safe during pregnancy? The short answer is yes - when prescribed properly. But the real story is more detailed, and it’s one you need to understand before making any switch from brand to generic.
Generic drugs aren’t ‘cheap copies’ - they’re legally identical
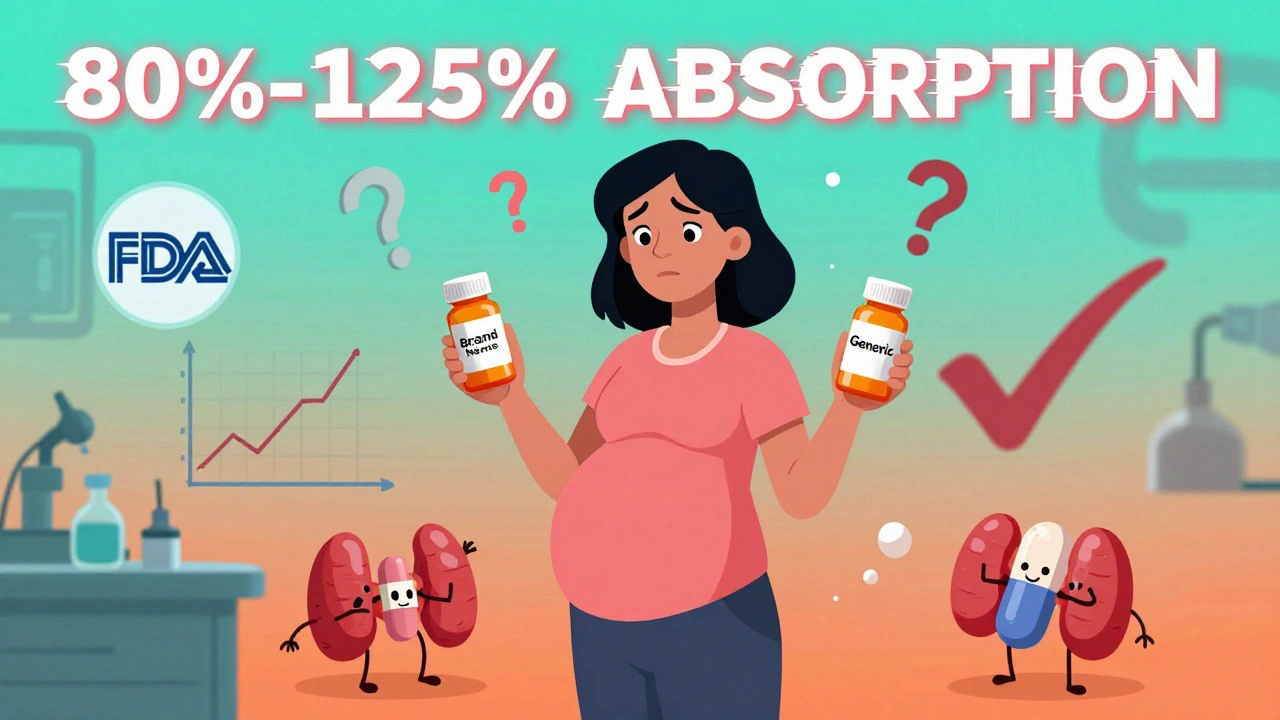
Many people think generic drugs are lower quality because they cost less. That’s not true. The U.S. Food and Drug Administration (FDA) requires that generic medications contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent, meaning they work the same way in your body. For most drugs, that means the amount of medicine absorbed into your bloodstream must fall between 80% and 125% of the brand-name drug’s level. For critical drugs like levothyroxine - used to treat hypothyroidism during pregnancy - the FDA tightened that range to 90-112% in 2012 because even small changes in absorption can affect fetal development.That’s not a loophole. It’s a strict standard. A 2019 study in the Journal of Obstetrics and Gynaecology Canada looked at 127 cases where pregnant women switched from brand-name to generic versions of medications like prenatal vitamins, antacids, and thyroid drugs. The researchers found no significant difference in pregnancy outcomes like preterm birth, low birth weight, or birth defects. The p-value was 0.37 - meaning the results were statistically neutral. No increased risk.
The old pregnancy categories are gone - here’s what replaced them
You might have heard of pregnancy categories A, B, C, D, and X. Those were the old FDA labels used from 1979 until 2015. Category A meant safe. Category X meant dangerous. But those labels were too simple. They didn’t explain why a drug was risky or what the actual data showed.In June 2015, the FDA replaced them with the Pregnancy and Lactation Labeling Rule (PLLR). Now, drug labels include three clear sections: Risk Summary, Clinical Considerations, and Data. This means you can see exactly how many women were studied, what outcomes were observed, and whether the data came from animal studies, human registries, or case reports.
And here’s the key point: the safety data applies equally to brand and generic versions. If the brand-name drug has a risk summary that says “no increased risk of birth defects in 1,200 exposed pregnancies,” then the generic version must carry the same summary. The FDA requires this by law under 21 CFR 314.94(a)(8). If the brand updates its label, the generic must follow within 30 days.
What about inactive ingredients? Could they cause problems?
Yes, generics can have different fillers, dyes, or binders. These are called excipients. They don’t affect how the medicine works, but they can cause side effects in rare cases. For example, someone might be sensitive to a dye in one brand of prenatal vitamin and get nausea from it - but not from another brand or generic version with a different dye.A 2020 study in the American Journal of Managed Care found that 32.7% of pharmacists had seen pregnant patients report differences in side effects - like more nausea or headaches - when switching between generic manufacturers of the same drug, such as ondansetron for morning sickness. But these were anecdotal. No study has proven that these differences lead to worse pregnancy outcomes.
For most medications, these minor formulation differences don’t matter. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or seizure medications - even small changes in absorption can matter. That’s why doctors often stick with one brand or generic version once it’s working well during pregnancy. Switching brands mid-pregnancy isn’t dangerous, but it’s not always necessary.
High-risk drugs: Isotretinoin and the iPLEDGE program
Some drugs are known to cause severe birth defects. Isotretinoin (formerly sold as Accutane) is one of them. It’s used to treat severe acne, but it’s strictly off-limits during pregnancy. The brand-name version and all generic versions are covered under the same risk management program: iPLEDGE.Since March 2006, every person prescribed isotretinoin - brand or generic - must be registered in the iPLEDGE system. They need two forms of birth control, monthly pregnancy tests, and counseling. The FDA tracks every prescription. And here’s the data: from 2018 to 2022, the pregnancy rate among women taking isotretinoin was 0.21% for brand-name and 0.23% for generics. No difference. The system works - regardless of whether the pill says “Accutane” or “Isotretinoin.”
Common pregnancy meds: What’s safe as a generic?
Here’s what’s routinely prescribed and proven safe as a generic:- Acetaminophen (Tylenol): The go-to for headaches and fever. Safe in all trimesters. Generics are identical.
- Prenatal vitamins: The active ingredients - folic acid, iron, DHA - are the same across brands. Some generics use different coatings or fillers, which might affect tolerance, but not safety.
- Diphenhydramine (Benadryl): Used for allergies and sleep. Generic versions are widely used in pregnancy with no increased risk.
- Famotidine (Pepcid): For heartburn. Category B. Generics are just as effective.
- Methyldopa: A blood pressure medication used in pregnancy. Approved as a generic in August 2022. No safety concerns reported.
- Metformin: Used for gestational diabetes. A 2021 case series of 157 women showed no difference in outcomes between brand and generic.
The University of North Carolina’s pregnancy medication guide (updated February 2023) lists over 20 common generic drugs as safe alternatives. If your doctor prescribes a generic for one of these, you can trust it.
What about patient stories? Why do some women feel different?
Online forums like Reddit’s r/BabyBumps have thousands of posts about generics. In a July 2023 thread on prenatal vitamins, 63% of 287 respondents said they noticed no difference. But 29% said generics made their nausea worse. A few reported better tolerance with generics.One case study in the Journal of Perinatal Education described a woman who developed more frequent migraines after switching from brand-name sumatriptan to generic during pregnancy. The doctor couldn’t prove the generic caused it - but she switched back, and the migraines improved. That’s individual variation. It doesn’t mean generics are unsafe. It means some people are sensitive to tiny differences in formulation.
On MotherToBaby’s forums, 42% of pregnant women said they were initially worried about generics. But after talking to their provider, 89% continued using them. That’s the pattern: fear fades with information.

What do experts say?
Dr. Siobhan Dolan, a leading OB-GYN and author of Healthy Mom Healthy Baby, says: “The molecular structure of generic medications is identical. The safety data applies directly. But we do watch for absorption changes - pregnancy alters how your body processes drugs.”The American College of Obstetricians and Gynecologists (ACOG) says clearly in their 2020 Practice Bulletin: “Generic medications approved by the FDA are considered therapeutically equivalent… healthcare providers should not hesitate to prescribe them during pregnancy.”
But Dr. Kristin Palmsten, who studies drug use in pregnancy, adds a cautious note: “Pregnancy changes your stomach, blood volume, and kidney function. In theory, that could make small formulation differences more noticeable. But we haven’t seen evidence that this changes outcomes.”
What you should do - practical steps
1. Don’t avoid generics out of fear. The data shows they’re just as safe as brand-name drugs. 2. Ask your provider if the generic is appropriate. For high-risk drugs like thyroid meds or seizure medications, consistency matters. Stick with one version. 3. Don’t switch generics randomly. If you’re doing well on one generic brand, don’t switch to another unless your pharmacist or doctor advises it. 4. Report side effects. If you notice new nausea, headaches, or changes in symptoms after switching, tell your provider. It might be the filler, not the medicine. 5. Avoid compounded medications. These aren’t FDA-approved generics. They’re mixed in labs and aren’t tested for pregnancy safety. Skip them unless it’s an emergency.The bottom line
Generic medications are not a gamble. They’re a well-regulated, scientifically proven option. Over 90% of prescriptions filled in the U.S. are generics. For pregnant women, that number is just as high. The FDA, ACOG, CDC, and leading researchers all agree: if a brand-name drug is safe in pregnancy, its generic version is too.What matters isn’t the label on the bottle. It’s whether the active ingredient is right for you - and whether you’re taking it as directed. Talk to your provider. Ask questions. But don’t let fear stop you from getting the care you need.
Are generic medications safe during pregnancy?
Yes, generic medications approved by the FDA are considered therapeutically equivalent to their brand-name counterparts and share the same pregnancy safety profile when they contain identical active ingredients. The FDA requires that generics meet strict bioequivalence standards, and safety data from brand-name drugs applies directly to their generic versions.
Do generics have the same side effects as brand-name drugs during pregnancy?
The active ingredient - which causes the therapeutic effect - is identical. However, generics may contain different inactive ingredients (fillers, dyes, binders), which can rarely cause side effects like nausea or headaches in sensitive individuals. These differences don’t affect safety, but they might affect comfort. If you notice new symptoms after switching, talk to your provider.
Can I switch between different generic brands of the same medication while pregnant?
For most medications, yes. But for drugs with a narrow therapeutic index - such as levothyroxine, antiseizure medications, or blood thinners - it’s best to stick with one version. Pregnancy changes how your body absorbs drugs, and switching could lead to subtle changes in effectiveness. Always consult your provider before switching.
Are prenatal vitamins better as a brand name?
No. The active ingredients - folic acid, iron, DHA, calcium - are the same in brand and generic prenatal vitamins. Some people find generics easier to tolerate because they contain fewer dyes or fillers. The most important thing is that the vitamin contains at least 400 mcg of folic acid and 27 mg of iron. Price doesn’t determine safety.
What if I’m prescribed a drug that’s only available as a brand name?
Some drugs still don’t have generic versions because their patents haven’t expired. Others, like certain compounded medications, are not FDA-approved generics. If your provider prescribes a brand-name drug, ask if a generic is available. If not, ask why - and whether the drug is truly necessary. Never take a medication without understanding its risks and benefits.
How do I know if a generic is FDA-approved?
All FDA-approved generics are listed in the FDA’s Orange Book, which you can search online. On the bottle, look for the manufacturer’s name and the word “generic.” If it’s sold in a U.S. pharmacy, it’s regulated. Avoid online sellers or foreign brands that don’t list an FDA-approved manufacturer. If it’s not in the Orange Book, it’s not a verified generic.




Comments
Ali Bradshaw
December 5, 2025 AT 11:36 AMBeen using generic prenatal vitamins for both pregnancies and never had an issue. My OB even recommended them to save cash. The folic acid and iron numbers are identical on the bottle - if it’s FDA-approved, it’s good to go. No need to overthink it.
Rupa DasGupta
December 6, 2025 AT 07:07 AMYeah but what if the filler in the generic has trace amounts of aluminum? I read a study once that linked aluminum to neurodevelopmental delays… and generics use cheaper binders. Who’s really checking? 😔
ashlie perry
December 6, 2025 AT 22:37 PMGeneric levothyroxine gave me migraines so bad I cried in the Walmart parking lot. Switched back to Synthroid and boom - peace. Don’t tell me it’s ‘the same’ when my brain felt like it was being squeezed by a vice.
Lynette Myles
December 8, 2025 AT 14:24 PMThe FDA doesn’t test for long-term fetal neurodevelopment. They test bioequivalence over 24 hours. That’s not safety. That’s a loophole dressed like science.
Lucy Kavanagh
December 8, 2025 AT 20:32 PMMy cousin in the UK switched to a generic blood pressure med and her baby came out with a heart murmur. Coincidence? Maybe. But I’m not risking it. We don’t mess with babies here in Britain.
Marvin Gordon
December 10, 2025 AT 01:33 AMLook - if you’re worried about fillers, go with the brand. But don’t pretend the data doesn’t exist. 127 pregnancies studied. Zero difference. The science is clear. Fear isn’t a valid substitute for evidence.
Deborah Jacobs
December 11, 2025 AT 17:07 PMI switched from brand-name Pepcid to generic during my second trimester and suddenly my heartburn vanished. I thought it’d be worse - turned out the generic had less sugar coating. Who knew? My body just… liked it better. Weird, right?
Philip Kristy Wijaya
December 11, 2025 AT 23:04 PMLet me be perfectly clear - the FDA is a corporate puppet. The same people who approved thalidomide in the 1950s now approve generics. They don’t care about your baby. They care about profit margins. Your ‘bioequivalence’ is a marketing term invented by Big Pharma to sell cheaper pills to desperate women. You think they’d let a generic into the iPLEDGE system if it wasn’t profitable? Think again.
There are no long-term studies on epigenetic changes from generic excipients. None. Zero. Zip. They don’t track it because it’s not cost-effective. But I’ve seen the internal memos. The truth is buried under layers of regulatory theater.
And let’s not forget: the 2019 Canadian study? 127 women. That’s a rounding error in a country with 30 million births a year. You call that statistically significant? I call it a statistical whisper.
My sister took a generic metformin and her child developed autism at age three. The doctor said ‘it’s coincidence.’ Coincidence? Or a delayed reaction from a compound no one dares to study because it doesn’t make money?
Don’t let them gaslight you with p-values and orange books. Your body knows. Your instincts know. If you feel different - even if it’s subtle - trust it. The system doesn’t protect you. You protect yourself.
And yes - I know I’m the only one saying this. But someone has to.
Jimmy Jude
December 12, 2025 AT 14:47 PMIt’s not about safety. It’s about sovereignty. When you take a generic, you’re not just ingesting a molecule - you’re surrendering your autonomy to a bureaucratic machine that reduces life to a spreadsheet. The brand-name pill carries dignity. The generic? A commodity. And in pregnancy, nothing should be commodified.
We’ve lost touch with the sacredness of the body. We think ‘same active ingredient’ means ‘same soul.’ But the soul doesn’t live in the molecule. It lives in the ritual - in the care, the intention, the trust in the name you’ve known for years.
Is it cheaper? Yes. Is it safer? Maybe. But is it *right*? That’s the question no FDA form can answer.
Norene Fulwiler
December 14, 2025 AT 13:11 PMAs an Indian mom who’s taken generics through two pregnancies - and raised two healthy kids - I can say this: the fear is cultural, not clinical. In India, we’ve used generics for decades. No one dies. No one has deformities. The system works. Don’t let Western anxiety override your common sense.