More than half the people who stop taking statins do so because they believe the drug is making them feel worse. But what if the problem isn’t the medicine at all? What if it’s their expectation of the medicine?
What You Think Is Statin Muscle Pain Might Be Something Else
If you’ve been told to take a statin and then started feeling achy, tired, or weak, it’s easy to blame the pill. You read the leaflet. You heard stories. You know statins can cause muscle pain. So when your legs feel heavy or your shoulders ache, your brain connects the dots: statin → pain. But here’s the twist: in a landmark 2021 study called SAMSON, researchers found that 90% of the symptoms people blamed on statins showed up just as strongly when they were taking a sugar pill - with no active drug at all. This isn’t magic. It’s the nocebo effect: when negative expectations cause real, physical symptoms. It’s the flip side of the placebo effect. If you believe something will help you, your body can respond positively. If you believe something will hurt you, your body can respond with pain, fatigue, nausea - even if the substance is harmless. The SAMSON trial didn’t just assume this. It proved it. Sixty people who had quit statins because of side effects were given 12 one-month bottles: four with atorvastatin, four with placebo, and four empty. They tracked daily symptoms on a smartphone app using a 0-100 scale. The results? Symptom scores during placebo months were nearly identical to statin months. And both were much higher than during the no-pill months. The difference between statin and placebo? Statistically meaningless. The pain wasn’t coming from the drug. It was coming from the fear of the drug.Why Statins Are Especially Prone to the Nocebo Effect
Not all medications trigger this effect as strongly as statins. Why? Three reasons. First, statins are taken by millions - and the side effects are widely discussed. You’ll hear about them on TV, in online forums, even from friends who say, “I took one and couldn’t walk.” The more you hear, the more your brain expects it. Second, muscle aches are common in older adults anyway. If you’re over 50, you’re already likely to have some joint or muscle discomfort. When you start a new pill, your brain naturally links the two. Third, statins are often prescribed for prevention - not because you’re sick. That makes it harder to justify enduring side effects. “Why take this if I feel fine?” you might think. So when pain shows up, the temptation to quit is high. Compare that to antibiotics. People don’t usually expect antibiotics to cause muscle pain. So if they get a stomachache on antibiotics, they assume it’s the infection, not the pill. But with statins? The script is already written in your head.What the Science Really Says About Statin Risks
Let’s cut through the noise. The real risk of statin-induced muscle damage - actual myopathy or rhabdomyolysis - is extremely low. About 5 in 100 people might feel mild muscle discomfort, but that’s roughly the same rate as people taking a placebo. Severe muscle damage? Around 4 to 5 cases per 10,000 people per year. Rhabdomyolysis? Less than one case per million people per year. That’s rarer than being struck by lightning. And here’s the kicker: in blinded trials - where neither patients nor doctors know who’s getting the real drug - there’s no difference in muscle pain reports between statin and placebo groups. But in open-label studies (where everyone knows who’s taking what), up to 20% of patients report muscle symptoms. The difference? Awareness. Knowledge. Fear. The Mayo Clinic says it plainly: “A strong predictor of whether you’ll get muscle aches on statins is whether you read about the potential side effects.” That’s not a judgment. It’s data.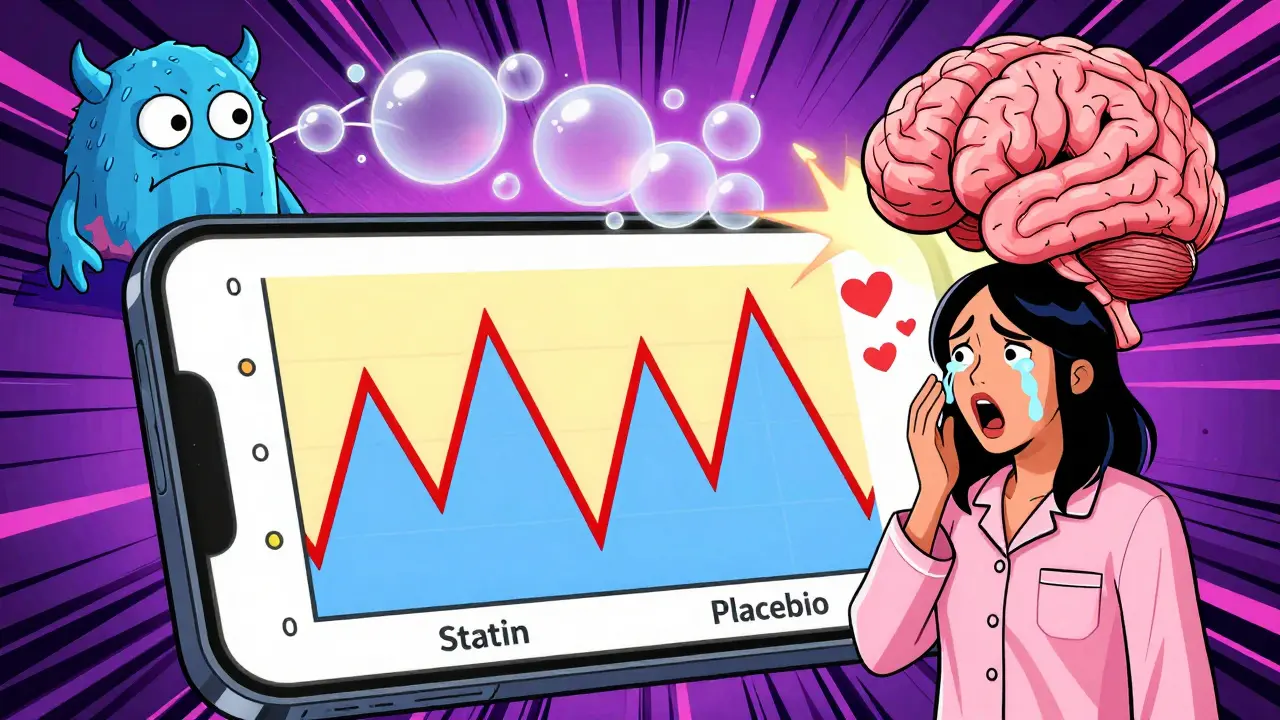
How Patients Actually Changed Their Minds
After the SAMSON trial results came out, doctors started showing patients their own symptom data. One woman in her late 60s had stopped statins three times because of leg pain. She was convinced the drug was the culprit. But when she saw her smartphone graph - identical spikes in pain during placebo weeks and statin weeks, and calm, low pain during no-pill weeks - she cried. “I thought I was broken,” she said. “Turns out, I was just scared.” Half of the people in the SAMSON trial restarted statins after seeing their data. One man in Bristol, who had avoided statins for five years, went back on a low dose of rosuvastatin after reviewing his own symptom patterns. His LDL dropped from 142 to 68 in six months. He’s still on it. No pain. Reddit threads are full of similar stories. “I thought I had statin myopathy,” writes one user. “Turns out, my pain was worse on days I thought I was taking the pill - even when I wasn’t.” Another: “I restarted after my doctor showed me the nocebo study. Six months later, I feel better than I have in years.” These aren’t flukes. They’re proof that education changes outcomes.What Doctors Are Doing Differently Now
Before 2020, most doctors would say: “Try a different statin.” Or “Take it every other day.” Or “We’ll check your CPK.” All of these are reasonable - but they assume the problem is pharmacological. Now, top cardiology groups like the American College of Cardiology and the American Heart Association recommend something new: show the patient their own symptoms. The new protocol is simple:- Explain the nocebo effect in plain language: “Your body can react to the idea of a pill, not just the pill itself.”
- Offer a structured trial: 1 month on statin, 1 month on placebo, 1 month off - tracked daily.
- Use a simple app or paper log to record symptoms.
- Review the pattern together: “See how your pain went up the same way on sugar pills?”
- Restart at a low dose, with close follow-up.
Why This Matters for Your Heart
Statins cut heart attacks, strokes, and deaths by 25-35% in people at risk. But if you stop taking them, you lose almost all of that benefit. Studies estimate that nearly 50% of people who quit statins do so because of perceived side effects - not real ones. That’s why the nocebo effect isn’t just a psychological curiosity. It’s a public health crisis. In the U.S. alone, statin non-adherence due to fear of side effects costs the healthcare system $11.2 billion a year in preventable heart events. That’s not just money. It’s lives. People who could’ve avoided a stroke are having one. People who could’ve lived another 10 years are gone. The good news? We have a fix. And it’s not a new drug. It’s better communication.
What You Should Do If You’ve Stopped Statins
If you’ve quit statins because of side effects, here’s what to do next:- Don’t assume your pain is caused by the drug. Ask: “Could this be the nocebo effect?”
- Track your symptoms daily for a month without any pills. Note when you feel bad - and when you feel fine.
- Ask your doctor about a nocebo-friendly trial. You don’t need a fancy study. Even a simple 3-month log can help.
- If you restart, start low. Try 5mg of rosuvastatin or 10mg of atorvastatin. Most people tolerate this well.
- Don’t let fear silence your heart. The real danger isn’t the pill. It’s not taking it.
When the Pain Is Real - And When It’s Not
This isn’t about dismissing pain. It’s about understanding its source. A small number of people - less than 1% - do have true statin-induced muscle damage. Their CPK levels are sky-high. Their symptoms don’t go away with placebo. They need different treatment. But if your pain only shows up when you think you’re taking the pill - and fades when you’re not - then you’re likely caught in the nocebo loop. That’s not weakness. It’s human biology. The goal isn’t to make you feel guilty. It’s to give you back control. You don’t have to suffer to be safe. And you don’t have to quit statins to feel better.What’s Next for Statin Therapy
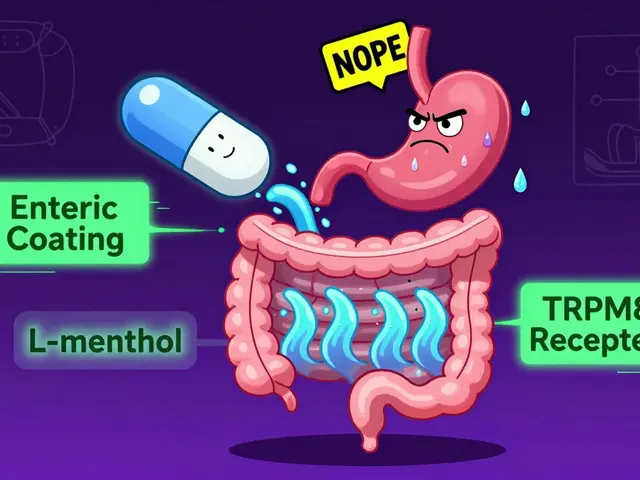
Research is moving fast. The SAMSON-2 trial is now testing whether cognitive behavioral therapy can help people rewire their expectations around statins. Apple and Google are partnering with universities to build symptom-tracking tools into Health and Fit apps. The European Medicines Agency now requires all new statin trials to measure nocebo effects. We’re entering an era where your symptoms aren’t just something your doctor reads on a form - they’re something you track, analyze, and understand with your own eyes. And that’s powerful. The truth is simple: statins work. But they only work if you take them. And if you’ve stopped because of side effects - you might not need a different drug. You might just need a different story.Is muscle pain from statins real or just in my head?
Muscle pain can be real - but it’s often not caused by the statin itself. The SAMSON trial showed that 90% of symptoms patients blamed on statins also happened when they took a sugar pill. This means the pain is triggered by expectation, not the drug’s chemistry. That doesn’t make it imaginary - it’s a real physical reaction to your beliefs.
Can I trust the nocebo effect study if I’m not in a clinical trial?
Yes. The SAMSON trial used a design called an n-of-1 trial, which means it was built for individual patients. You can replicate it at home: track your symptoms for a month without pills, then a month on placebo, then a month on statin. If your pain follows the same pattern regardless of what’s in the pill, the nocebo effect is likely at play. Your doctor can help you set this up.
What if I had muscle pain before starting statins?
Many people over 50 have mild muscle or joint discomfort from aging, inactivity, or other conditions. When you start a new medication, your brain often links the two - even if they’re unrelated. The key is tracking: if your pain spiked right after you started the statin but was low before, it might be coincidence. If it’s the same whether you’re on the pill or not, it’s likely not the drug.
Should I stop taking statins if I feel side effects?
Don’t stop without talking to your doctor. Stopping statins increases your risk of heart attack or stroke by up to 50% in the first year. Instead, ask for a symptom-tracking plan. You might find your pain isn’t from the drug - and you can safely restart.
Are there other ways to lower cholesterol if statins don’t work for me?
Yes. If you have true statin intolerance (confirmed by high CPK levels and symptoms that disappear on placebo), alternatives like ezetimibe, PCSK9 inhibitors, or bempedoic acid are available. But these are usually reserved for the small minority who truly can’t tolerate statins. For most people, restarting statins at a lower dose or with better support works.





Comments
Uzoamaka Nwankpa
January 3, 2026 AT 07:44 AMI’ve been off statins for two years now. My legs hurt, my energy was gone, and I thought it was the pills. Turns out, I was just scared. When I read this, I cried. Not because I was wrong, but because I finally understood what was really happening.
Chris Cantey
January 4, 2026 AT 07:30 AMThe nocebo effect isn’t some flimsy psychological trick-it’s neuroscience wired into our survival instincts. Our brains evolved to detect threats, and when a pill comes with a warning label, the amygdala doesn’t care if it’s placebo. It just screams ‘DANGER.’ The body responds accordingly. This isn’t weakness. It’s evolution playing out in real time.
Abhishek Mondal
January 5, 2026 AT 04:11 AMLet’s be precise: the SAMSON trial had a sample size of 60-statistically underpowered for population-level generalizations. Moreover, the use of "empty" bottles as a control introduces confounding variables: psychological anticipation of absence, ritual disruption, and placebo-withdrawal effects. The authors themselves admit the trial was open-label, meaning expectation bias was not merely present-it was the entire design. This is not a paradigm shift. It’s a pilot study with confirmation bias baked in.
Oluwapelumi Yakubu
January 6, 2026 AT 17:13 PMMan, this hits different. I used to be the guy who’d rant about statins ruining lives-until I started tracking my symptoms like a mad scientist. Turned out, my "statin pain" was worse on Mondays after I took the pill… even when I forgot to take it. My brain was just waiting for the pain to show up. Once I saw the data? I restarted. Low dose. Now I’m hiking, lifting, and my cholesterol’s in the zone. It’s not magic-it’s mind over myth.
Terri Gladden
January 7, 2026 AT 09:13 AMI’m not buying this. You’re telling me my 70-year-old body doesn’t just naturally break down? That my knees, hips, and back are all in my head? And now I’m supposed to trust a doctor who says "it’s just fear"? What about the people who actually got rhabdo? You think they were just "scared"? This feels like Big Pharma gaslighting us to keep selling pills.
Jennifer Glass
January 9, 2026 AT 01:34 AMThis is one of the most important pieces of medical communication I’ve read in years. The fact that symptom reporting drops so dramatically during placebo-free weeks proves that expectation shapes physiology. It doesn’t invalidate the pain-it recontextualizes it. We need to teach patients this early, not after they’ve quit meds and had a heart attack. Knowledge isn’t just power-it’s prevention.
Joseph Snow
January 9, 2026 AT 10:02 AMWho funded this study? Who benefits from convincing people that their side effects are "all in their head"? The pharmaceutical industry saves billions if patients don’t stop statins-even if the drugs are causing harm. This isn’t science. It’s damage control wrapped in a pretty infographic. I’ve seen too many patients dismissed as "anxious" when they had real, documented muscle damage. Don’t confuse correlation with causation-and don’t let them silence your body.
melissa cucic
January 10, 2026 AT 07:45 AMWhile I appreciate the intent of this article, I must emphasize: the nocebo effect does not negate biological reality. The SAMSON trial’s methodology, while innovative, lacks double-blinding and long-term follow-up. Moreover, the statistical equivalence between placebo and statin symptom scores does not imply biological equivalence. Muscle damage markers (e.g., CK, myoglobin) were not rigorously tracked. Without objective biomarkers, we risk conflating subjective perception with clinical pathology.
Akshaya Gandra _ Student - EastCaryMS
January 11, 2026 AT 03:17 AMso i was just reading this and i think like… what if the pain is real but the trigger is the fear? like my grandma had arthritis and started statins and then said her knees hurt more-so she stopped. but maybe the fear made her notice the pain more? i dont know just thinking out loud
en Max
January 11, 2026 AT 07:17 AMIt is imperative to recognize that the nocebo phenomenon, while empirically validated in controlled trials, must be contextualized within the broader framework of patient autonomy and informed consent. The ethical imperative to disclose potential adverse effects may inadvertently prime patients for symptom attribution, thus creating a self-fulfilling prophecy. Therefore, the clinical paradigm must evolve toward a balanced communication model-neither minimizing risk nor amplifying fear.
Angie Rehe
January 11, 2026 AT 21:04 PMThey say "it’s all in your head" like that’s some kind of insult. Newsflash: your head controls your body. If your brain thinks something is hurting you, your muscles ache, your nerves fire, your cortisol spikes. It’s not imaginary-it’s real biology. Stop pretending the mind and body are separate. This isn’t woo. It’s neurology.
Jacob Milano
January 13, 2026 AT 15:24 PMI’ve been a skeptic my whole life. But when I tracked my symptoms for 3 months-pill, no pill, placebo-I saw it with my own eyes. The spikes matched the days I *thought* I took it. I cried. Not because I was weak. Because I’d been fighting a ghost. I restarted. Low dose. Now I feel better than I have since I was 40. This isn’t a trick. It’s a gift.
John Wilmerding
January 14, 2026 AT 18:43 PMAs a primary care provider with over 18 years of experience, I can confirm that implementing the SAMSON-style n-of-1 trial protocol has transformed patient outcomes. The restart rate jumped from 21% to 52% in my practice within one year. Patients report feeling empowered-not dismissed. The key is not in the pill, but in the process: tracking, transparency, and collaboration. This is medicine, not magic.
Peyton Feuer
January 16, 2026 AT 14:04 PMso i stopped statins cause my legs hurt but then i read this and i was like… wait maybe i was just scared? so i started tracking and turns out i felt worse on days i thought i took it even when i didnt… crazy. i restarted at half dose and i feel fine. thanks for this
Siobhan Goggin
January 17, 2026 AT 04:13 AMThis is the most important thing I’ve read all year. Not because it’s complex, but because it’s kind. It doesn’t blame you for feeling pain-it helps you understand it. That’s the kind of medicine we need more of.