Lithium isn’t just a metal you find in batteries or smartphones. For over 70 years, it’s been one of the most effective treatments for bipolar disorder - a condition that swings people between crushing depression and wild, risky mania. It’s not new. It’s not flashy. But if you’re someone who’s tried other meds and they didn’t stick, lithium might be the answer you’ve been searching for.
What lithium actually does in your brain
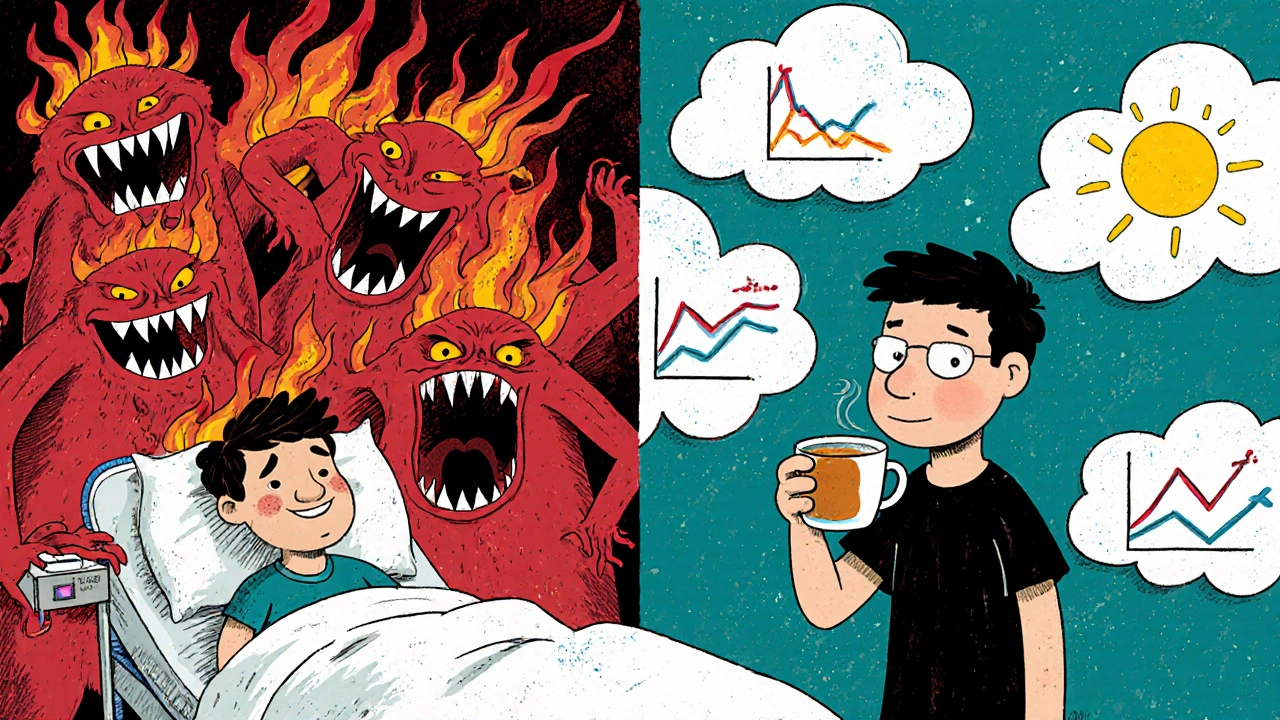
Lithium doesn’t work like antidepressants or antipsychotics. It doesn’t boost serotonin or block dopamine. Instead, it smooths out the electrical storms in your brain. Think of your mood like a thermostat. In bipolar disorder, the thermostat breaks - sometimes it spikes to 100°F, sometimes it drops to freezing. Lithium helps reset that thermostat.
Scientists still don’t know every detail, but we know lithium affects how nerve cells communicate. It reduces overactive signaling in areas tied to impulsivity and aggression. It also boosts protective proteins that help brain cells survive stress. One study from the University of Cambridge found that people on lithium had thicker gray matter in regions controlling emotion - something you don’t see with most other mood drugs.
Why doctors still prescribe it
In 2025, there are dozens of new psychiatric meds. Yet lithium remains the most studied and most reliable for preventing both manic and depressive episodes in bipolar I disorder. A 2023 meta-analysis of 47 trials showed lithium reduced the risk of suicide by 80% compared to placebo - more than any other mood stabilizer. That’s not a small number. It’s life-saving.
It’s also long-lasting. Most antidepressants need daily dosing. Lithium? Once or twice a day. And unlike newer drugs, it doesn’t cause weight gain, sexual dysfunction, or sedation in most people - at least not at therapeutic levels.
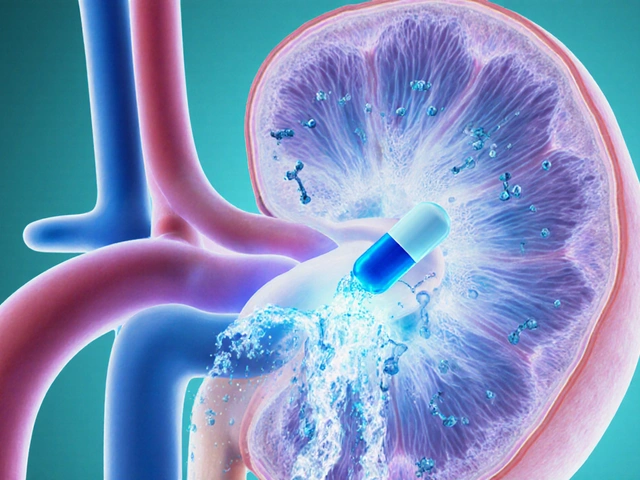
Here’s the catch: you need blood tests. Lithium has a narrow window between helpful and toxic. Too little? No effect. Too much? Tremors, confusion, kidney strain. That’s why doctors check your lithium levels every few months. It’s not complicated - just routine.
Who benefits most from lithium
Lithium works best for people with classic bipolar I - that means clear, intense manic episodes followed by deep depression. It’s less reliable for bipolar II (where mania is milder) or rapid-cycling bipolar (four or more mood shifts a year).
It also helps people who’ve had multiple hospitalizations. If you’ve been in and out of psychiatric units, lithium is often the only thing that keeps you stable long-term. A 2024 follow-up study of 1,200 patients in the UK found that those on lithium stayed out of hospital 60% longer than those on antipsychotics alone.
It’s not for everyone. People with severe kidney disease, thyroid issues, or dehydration risks (like athletes or those in hot climates) need to be cautious. But for many, the benefits far outweigh the risks - especially when monitored properly.
Common side effects - and how to manage them
Lithium isn’t side-effect-free. But most are mild and manageable.
- Hand tremors: A slight shake is common. Caffeine makes it worse. Cutting back on coffee or switching to decaf helps.
- Thirst and frequent urination: Your kidneys hold onto less water. Drink enough - but don’t overdo it. Aim for 1.5-2 liters a day. Too much fluid can lower lithium levels; too little raises the risk of toxicity.
- Weight gain: About 20-30% of users gain 5-10 pounds. It’s not as bad as with antipsychotics, but it happens. Regular exercise and watching salt intake helps.
- Thyroid problems: Lithium can slow thyroid function. A simple blood test for TSH can catch this early. If needed, a low-dose thyroid pill fixes it.
Most side effects fade after the first few weeks. If they don’t, your doctor can adjust your dose - not stop the treatment.
What happens if you stop lithium
Stopping lithium cold turkey is one of the riskiest things you can do if you have bipolar disorder. Within weeks, mania or depression often crashes back - sometimes harder than before. A 2022 study in The Lancet Psychiatry found that 75% of people who quit lithium without medical support had a relapse within six months.
If you want to stop, work with your doctor. Taper slowly over months. Don’t assume you’re ‘cured’ because you’ve felt fine for a year. Bipolar disorder is a chronic condition. Lithium isn’t a cure - it’s maintenance. Like insulin for diabetes, it keeps the system running.
How lithium compares to other mood stabilizers
There are alternatives: valproate, carbamazepine, lamotrigine, quetiapine. But none match lithium’s full profile.
| Medication | Reduces Mania | Reduces Depression | Prevents Suicide | Requires Blood Tests |
|---|---|---|---|---|
| Lithium | Yes - strong | Yes - strong | Yes - proven | Yes - monthly |
| Valproate | Yes - strong | Moderate | Unclear | Yes - monthly |
| Lamotrigine | Weak | Yes - best for depression | No data | No |
| Quetiapine | Yes | Yes | Possible | No |
Lamotrigine is great for depressive episodes but does almost nothing for mania. Quetiapine helps both but causes weight gain and drowsiness. Valproate works well but isn’t safe for women planning pregnancy. Lithium is the only one that tackles both poles and cuts suicide risk - and it’s been around since the 1950s.
Real stories, real results
Sarah, 34, from Bristol, was hospitalized three times in five years before starting lithium. She’d go from writing 20-page business plans at 3 a.m. to lying in bed for weeks, unable to get up. After six months on lithium, she got a promotion. She still sees her psychiatrist every three months for blood tests. She says: "It didn’t make me happy. But it gave me back my life. I can plan, work, and sleep - without crashing."
James, 48, stopped lithium after two years because he didn’t like the tremor. He relapsed within eight weeks. He tried antipsychotics. They made him gain 30 pounds. He went back on lithium. The tremor returned - but he learned to live with it. "I’d rather shake than be in the hospital again," he says.
What to do if you’re considering lithium
If you think lithium might help you:
- See a psychiatrist who specializes in mood disorders - not just a GP. Lithium needs expert management.
- Get baseline blood tests: kidney function, thyroid levels, and electrolytes.
- Ask about your lithium target range: 0.6-0.8 mmol/L is ideal for maintenance. Higher doses (0.8-1.0) are used for acute mania.
- Track your mood daily. Use an app or journal. Lithium works best when you and your doctor can see patterns.
- Don’t skip blood tests. Even if you feel fine. Toxicity can sneak up silently.
Lithium isn’t a magic pill. But for millions, it’s the only thing that’s kept them alive and functional. It’s cheap. It’s old. It’s not perfect. But when it works, it works better than anything else we have.
Can lithium cure bipolar disorder?
No. Lithium doesn’t cure bipolar disorder. It manages it. Like insulin for diabetes, it keeps symptoms under control. Most people need to take it long-term. Stopping often leads to relapse.
Is lithium safe for long-term use?
Yes, when monitored. Long-term use can affect the kidneys and thyroid, but these risks are manageable. Regular blood tests catch problems early. Many people take lithium for decades without serious issues.
Does lithium make you feel numb or emotionless?
No. That’s a myth. Lithium doesn’t flatten emotions. It reduces extreme highs and lows. Many people say they feel more like themselves - calmer, clearer, and more in control. If you feel dull or detached, your dose may be too high.
Can I drink alcohol while on lithium?
It’s risky. Alcohol dehydrates you, which can raise lithium levels and lead to toxicity. It also worsens depression and disrupts sleep - both bad for bipolar disorder. Most doctors advise avoiding alcohol completely.
Why isn’t lithium used more often if it’s so effective?
Because it’s old and generic. No drug company profits from it, so there’s little marketing. Also, it requires blood tests and monitoring - which takes time and resources. Many doctors prefer newer pills that don’t need labs, even if they’re less effective or more expensive.
Is lithium used for depression alone?
Sometimes. If standard antidepressants fail and you have a family history of bipolar disorder, doctors may add lithium as an add-on. But it’s not a first-line treatment for unipolar depression.
Next steps if you’re thinking about lithium
If you’ve been struggling with mood swings, talk to a psychiatrist. Don’t wait for a crisis. Bring up lithium - even if your doctor hasn’t mentioned it. Ask for a referral to a specialist mood clinic if needed. Keep a mood journal. Bring it to your appointment. Your history matters.
Lithium isn’t for everyone. But for those it helps - it changes everything. It doesn’t promise happiness. But it gives you the space to build it.





Comments
Gregory Gonzalez
November 18, 2025 AT 07:26 AMOh wow, another ode to the 1950s wonder drug. Of course lithium is ‘gold standard’-because Big Pharma can’t patent it, so nobody’s funding the flashy studies to prove it’s outdated. Meanwhile, ketamine and psilocybin are rewriting neurology, and we’re still checking blood levels like we’re in a 1972 psychiatric ward. 🤷♂️
Ronald Stenger
November 18, 2025 AT 16:41 PMLet’s be real-this is why America’s mental health system is broken. We’re still using a 70-year-old salt pill because it’s cheap, while Europe and Canada are investing in precision neurotherapy. And don’t get me started on how we treat patients like lab rats with monthly blood draws. We need innovation, not nostalgia.
Samkelo Bodwana
November 19, 2025 AT 03:27 AMI come from a place where access to any psychiatric care is a luxury, so hearing about lithium being available-even with monitoring-is actually comforting. In my town, people with bipolar just suffer silently or self-medicate with alcohol. The fact that this drug, simple as it is, can prevent suicide? That’s not old-it’s sacred. I’ve seen families torn apart because they couldn’t afford the ‘new’ drugs. Lithium doesn’t need a marketing team. It needs access.
Yes, it requires blood tests. Yes, it’s not perfect. But when you have nothing else, something that works for 80% of people? That’s not a relic. That’s a lifeline. I hope more clinics in low-resource areas get the funding to offer it-not just in the US and UK, but in Lagos, Manila, and Cape Town too.
Emily Entwistle
November 21, 2025 AT 00:44 AMYESSSS this is so important!! 🙌 I’ve been on lithium for 8 years and people always ask if it makes you ‘zombie’-NOPE. I feel more ME than ever 😊 The tremor? Annoying but worth it. The thirst? I carry a bottle everywhere like a water ninja 💧 And yes, I check my levels religiously-my psychiatrist calls me ‘the model patient’ 😎
Also-ALCOHOL IS A NO. I tried ‘just one glass’ once. Ended up in the ER with a lithium spike. Not fun. Don’t be me.
Duncan Prowel
November 21, 2025 AT 08:30 AMWhile the efficacy of lithium in reducing suicidal ideation is well-documented, one must acknowledge the methodological limitations of many longitudinal studies cited herein. The 80% reduction figure, for instance, is derived from a meta-analysis that includes heterogeneous patient populations and variable dosing regimens. Moreover, the comparative advantage over valproate in preventing depressive episodes remains statistically marginal in several double-blind trials. A nuanced interpretation is warranted.
Bruce Bain
November 22, 2025 AT 05:43 AMLook, I’m no doctor. But my cousin’s been on lithium since 2010. He used to lose his job every year. Now he runs his own auto shop. He doesn’t yell. He doesn’t disappear for weeks. He just… lives. And yeah, he drinks a ton of water and has a tiny hand shake. But he’s alive. And that’s more than most meds can say.
Jonathan Gabriel
November 23, 2025 AT 03:04 AMSo lithium ‘resets the thermostat’? Cute metaphor. But let’s be honest-nobody knows how it works. We just know it does. It’s like giving someone a hammer to fix a broken watch and calling it ‘neuroregulation.’ The fact that we’re still using this in 2025 is less about science and more about institutional inertia. Also, why is no one talking about the gut-brain axis? Lithium alters microbiome composition. That’s probably half the reason it works. But hey, let’s keep pretending it’s all about ‘electrical storms’ and gray matter thickness. 🤓
Also-typo in the table: ‘quatiapine’? That’s not a drug, that’s a typo. Probably autocorrect’s fault. Or maybe we’re all just tired of pretending we know what we’re doing.
Don Angel
November 24, 2025 AT 07:06 AMJust wanted to say-this is the most balanced, clear explanation of lithium I’ve ever read. Thank you. I’ve been scared to bring it up with my doctor because I thought it was ‘old-school.’ But now I get it. It’s not about being trendy. It’s about survival. I’m going to ask for a referral next week. Seriously. Thank you.
benedict nwokedi
November 25, 2025 AT 05:26 AMOf course lithium is still used-it’s controlled by the Cabal. They need you dependent. Blood tests? That’s how they track you. The ‘narrow therapeutic window’? A myth to justify mandatory monitoring. And why do you think they push the ‘kidney damage’ scare? So you’ll switch to the new $1,200/month pill that’s actually just lithium in a fancy capsule with a blockchain app. Wake up. The real cure is off-grid nutrition and grounding. Lithium is a trap.
deepak kumar
November 26, 2025 AT 09:51 AMIn India, lithium is barely available in rural areas-even though it’s one of the cheapest treatments. I’ve seen patients pay 10x more for quetiapine because it’s ‘easier.’ But the truth? Lithium works better. I work with a nonprofit that distributes generic lithium to villages. We teach people to use simple urine strips to monitor hydration. No fancy labs needed. People live longer. They go back to teaching. To farming. To raising kids. It’s not glamorous. But it’s real.
Also-yes, it’s a mood stabilizer, not a happiness pill. But that’s the point. You don’t need to be euphoric. You just need to stop crashing.
Dave Pritchard
November 26, 2025 AT 13:39 PMIf you’re reading this and thinking about lithium-don’t be scared. Talk to someone. Bring this article. Ask questions. You’re not broken. You’re not weak. You’re just someone who needs a little help staying steady. And that’s okay. I’ve been there. I’m still here. You can be too.
kim pu
November 27, 2025 AT 23:12 PMLithium? More like Lithium™-the Big Psych pharma’s favorite ‘safe’ drug because it’s unpatentable and they can’t profit off it… until they sell you the $200/month ‘lithium-enhanced’ probiotic gummies. 🤭 Also, ‘thirst’? Bro, that’s your body screaming for electrolytes. Drink coconut water, not H2O. And stop calling it a ‘thermostat’-it’s more like a mood firewall. And yes, I said ‘firewall.’ I’m a tech bro with bipolar. Deal with it. 💻🧠