When you’re managing a chronic condition like diabetes, high blood pressure, or arthritis, your medication isn’t just a pill you take once in a while-it’s part of your daily life. For many, that means taking five, ten, or even more pills every day. Sounds overwhelming? It is. And it’s not just about remembering to take them. It’s about staying safe while doing it.
Why Long-Term Medication Use Is Risky
Taking meds for years isn’t the problem. The problem is what happens when you’re taking too many at once, or when no one checks if they still make sense. This is called polypharmacy-taking five or more medications regularly. It’s common in older adults, but it’s not just an age thing. People with multiple chronic conditions-like heart disease, COPD, and depression-are often seeing different specialists, each prescribing their own drugs. No one’s looking at the big picture. The risks? Higher chance of side effects, falls, confusion, hospital visits, and even death. A study from the American Academy of Family Physicians found that people on five or more medications have a 30% higher risk of being hospitalized. And it’s not just the drugs themselves-it’s how they interact. For example, mixing aspirin and diclofenac can wreck your stomach lining. Taking opioids long-term without monitoring can lead to dependence, even if you’re not addicted.The 7 Rights of Safe Medication Use
Healthcare workers are trained on the 7 Rights to avoid mistakes. You should know them too. They’re not just for nurses-they’re your safety checklist.- Right patient: Are these pills really for you? Double-check the name on the bottle.
- Right drug: Does the label match what your doctor told you? Don’t assume.
- Right dose: Is it 5 mg or 50 mg? A decimal error can be deadly.
- Right route: Is it meant to be swallowed, applied to skin, or inhaled?
- Right time: Some meds work best in the morning. Others at night. Timing matters.
- Right documentation: Keep a written list of everything you take-including vitamins and supplements.
- Right reason and response: Why are you taking this? And have you noticed any new symptoms?
Keep a Medication List-And Update It
This is the single most powerful thing you can do. Write down every medication you take. Not just prescriptions. Include over-the-counter painkillers, herbal teas, magnesium supplements, and even daily aspirin. For each one, write:- Generic and brand name
- Dosage (e.g., 10 mg)
- How often (e.g., once daily, twice a day)
- Purpose (e.g., “for blood pressure,” “for joint pain”)
- When you started
Get a Medication Review Every Year
Your meds aren’t set in stone. Your body changes. Your conditions change. Your life changes. What helped you five years ago might be unnecessary-or even dangerous-now. Ask your GP or pharmacist for a full medication review at least once a year. They’ll go through your list and ask:- Is this still needed?
- Is there a safer alternative?
- Are any of these interacting badly?
- Are you actually taking them as prescribed?
Use Tools to Stay on Track
Memory fails. Life gets busy. That’s normal. But you don’t have to rely on willpower alone.- Pill organizers: Buy one with compartments for morning, afternoon, evening, and night. Fill it weekly.
- Smart reminders: Use your phone alarm, or apps like Medisafe or MyTherapy. They send alerts and even notify a family member if you miss a dose.
- Automatic refills: Many pharmacies offer free automatic refills with home delivery. No more running out.
- Barcode systems: If you’re in a hospital or care home, ask if they use barcode scanning to check your meds before giving them to you. It cuts errors by over half.
Watch for Red Flags
You don’t need to be a doctor to spot trouble. Pay attention to these signs:- Feeling dizzy or confused after starting a new med
- Unexplained bruising or bleeding
- Sudden weight gain or swelling
- Stomach pain, nausea, or black stools
- Slurred speech, muscle weakness, or falls
- Feeling worse instead of better
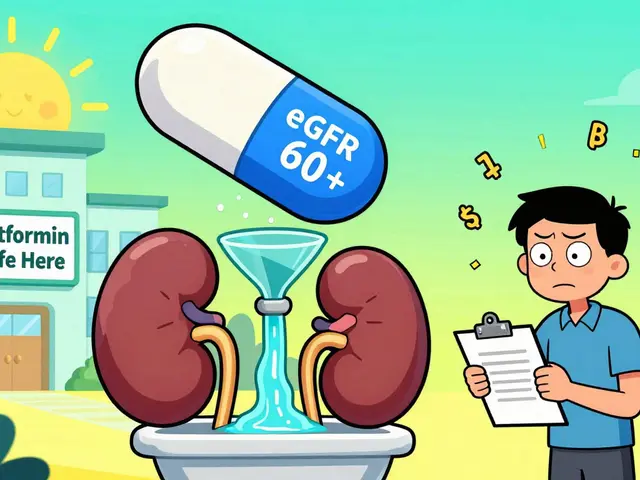
Cost Shouldn’t Stop You From Taking Your Meds
One in four people in the UK skip doses because they can’t afford them. That’s not just risky-it’s dangerous. But you don’t have to accept that.- Ask if there’s a generic version.
- Check if your pharmacy offers discount programs (like the NHS Low Income Scheme).
- Ask your doctor if a lower dose will work. Sometimes splitting pills (with approval) saves money.
- Use prescription savings cards-many are free and accepted at most pharmacies.

Involve Someone You Trust
You don’t have to do this alone. Find one person-a partner, child, friend-who knows your meds and can help. They can:- Remind you when to take pills
- Help you fill out your medication list
- Call the pharmacy when you’re out of refills
- Go with you to appointments and take notes
What If You Want to Stop a Med?
Some people stop meds because they feel fine. Or because they’re scared of side effects. Or because they think it’s “not working.” Don’t quit without talking to your doctor. Stopping blood pressure meds suddenly can cause a stroke. Stopping antidepressants cold turkey can trigger severe withdrawal. Even something like a steroid inhaler needs to be tapered down. Always ask: What happens if I stop this? What’s the safest way to stop? Your doctor should give you a plan-not just a yes or no.Final Thought: Your Meds Are Part of Your Health Story
Managing long-term meds isn’t about being perfect. It’s about being informed, involved, and vigilant. You’re not just a patient-you’re the lead in your own care team. The more you know about what you’re taking and why, the safer you’ll be. Don’t wait for a crisis to start asking questions. Start today. Write your list. Schedule your review. Talk to someone. Small steps add up to big safety gains.What should I do if I miss a dose of my chronic condition medication?
Don’t panic. Check the patient leaflet that came with your medication-it usually has instructions. If it doesn’t, call your pharmacist. For most drugs, if you miss a dose by a few hours, take it as soon as you remember. But if it’s close to your next dose, skip the missed one. Never double up unless your doctor says so. For blood thinners, diabetes meds, or heart drugs, even small mistakes can be risky, so always check.
Can I use herbal supplements with my prescription meds?
Some can be dangerous. St. John’s Wort, for example, can make blood pressure and antidepressant meds less effective. Garlic and ginkgo can increase bleeding risk if you’re on warfarin. Even common supplements like magnesium or calcium can interfere with antibiotics or thyroid meds. Always tell your doctor or pharmacist about every supplement you take-even if you think it’s “natural” or “harmless.”
Why do I need a medication review if I feel fine?
Feeling fine doesn’t mean your meds are still needed. Sometimes, your condition improves, and you don’t need the same dose-or any drug at all. Other times, side effects build up slowly. You might not notice you’re more tired, dizzy, or forgetful because it happened over months. A review catches these hidden risks before they become problems. It’s like a car service-you don’t wait until the engine fails.
How do I know if my meds are interacting badly?
Look for new symptoms that started after adding a new drug or changing a dose. Common signs: nausea, dizziness, confusion, unusual bruising, swelling in legs, or heart palpitations. If you’re on more than five meds, the risk goes up fast. Ask your pharmacist to run a drug interaction check. Most pharmacies have software that flags dangerous combinations. Don’t rely on memory-get it checked.
Is it safe to take my meds with alcohol?
For many chronic condition meds, the answer is no. Alcohol can make blood pressure drugs too strong, cause liver damage with statins, increase drowsiness with painkillers or antidepressants, and spike blood sugar in diabetics. Even one drink can be risky. If you drink, talk to your doctor. They may say it’s okay in small amounts-but never assume. When in doubt, skip it.
What if I can’t open my pill bottles?
You’re not alone. Arthritis or weak hands make this a real problem. Ask your pharmacist for easy-open caps, blister packs, or pre-filled pill organizers. Many pharmacies offer this service for free. You can also ask for liquid versions or patches if available. Never force the cap-risk of injury is real. Your safety matters more than keeping the original packaging.
Can my pharmacist help me with my medication plan?
Absolutely. Pharmacists are medication experts-and they’re more accessible than your doctor. They can check for interactions, explain side effects in plain language, help you set up reminders, and even call your doctor to suggest dose changes. Many NHS pharmacies now offer free Medicines Use Reviews (MURs). Book one if you’re on multiple long-term meds. It’s a 20-minute chat that could save your life.
How often should I update my medication list?
Update it every time something changes: a new prescription, a dose change, or if you stop a drug. Even if you just started a new vitamin. Keep the list current. Many people update it once a year-but that’s not enough. Set a reminder on your phone for the first of every month. It takes 2 minutes. That small habit prevents big mistakes.
What’s the biggest mistake people make with long-term meds?
Assuming they’re safe because they’ve been taking them for years. Just because a drug was right for you five years ago doesn’t mean it still is. Your body changes. Your health changes. New research comes out. The biggest danger isn’t forgetting to take your pills-it’s never asking if you still need them.
Are there free resources in the UK to help with medication safety?
Yes. The NHS offers free Medicines Use Reviews (MURs) for patients on multiple long-term medications. You can also get free prescription delivery through the NHS Low Income Scheme or Prescription Prepayment Certificate. Your local pharmacy may offer a home visit service if you’re housebound. And the NHS website has a free medication tracker tool you can download or print. Use them. They’re there for your safety.





Comments
Nishant Garg
January 17, 2026 AT 02:10 AMMan, I’ve been on six meds for my diabetes and hypertension for over a decade. I never thought about a yearly review until my pharmacist pulled me aside last year and said, ‘You’re taking two drugs that cancel each other out.’ Turned out I didn’t need the beta-blocker anymore-my BP stabilized after switching diets. That 20-minute chat saved me $400 a year and stopped my dizziness. Pharmacist = unsung hero.
Amy Ehinger
January 17, 2026 AT 18:12 PMI love how this post doesn’t just say ‘take your pills’-it actually gives you tools. My mom used to forget half her meds until we got her one of those pill organizers with the alarms. Now she calls me every Sunday to update her list. It’s not perfect, but it’s way safer than the old shoebox full of random bottles.
Ayush Pareek
January 17, 2026 AT 22:49 PMOne thing no one talks about enough: the mental load. Keeping track of all these meds isn’t just logistical-it’s exhausting. You start doubting yourself. ‘Did I take it?’ ‘Was that the blue one or the white one?’ Having a trusted person to double-check with isn’t a luxury-it’s a lifeline. I’m lucky my sister does this for me. No shame in needing help.
Sarah Mailloux
January 19, 2026 AT 21:35 PMJust started my meds list on my phone notes. Took 3 minutes. I’m gonna update it every time I refill something. No more guessing. Also, I asked my doc about generic lisinopril-saved me $120/month. Small win, big difference.
Crystel Ann
January 21, 2026 AT 15:14 PMMy grandma used to skip her blood thinner because she was scared of bleeding. She didn’t tell anyone. Then she fell and ended up in the ER with a brain bleed. Turns out she’d been taking ibuprofen for her knees-no one knew. This post? It’s the kind of thing that saves lives. Thank you for writing it.
Nat Young
January 22, 2026 AT 11:45 AMLet’s be real-most of these ‘safety tips’ are just corporate wellness fluff. The real issue is the healthcare system is broken. You’re supposed to remember 12 pills, keep a list, get a review, and not die? Meanwhile, your doctor sees you for 8 minutes a year. The burden shouldn’t be on patients-it should be on the system that’s overprescribing and under-coordinating.
Nicholas Urmaza
January 24, 2026 AT 08:49 AMPeople think they’re safe because they’ve been on the same meds for years. That’s the most dangerous myth out there. I’ve seen patients on statins for 15 years with no labs done. No liver checks. No cholesterol tracking. Just ‘I feel fine.’ Feeling fine doesn’t mean you’re not slowly destroying your kidneys. Get tested. Track it. Don’t assume.
Nilesh Khedekar
January 26, 2026 AT 00:15 AMOh here we go-another ‘take your pills’ lecture. Meanwhile, the pharmaceutical industry makes billions off polypharmacy. Why? Because they profit from you being dependent. They don’t want you to stop. They don’t want you to review. They want you to keep buying. Ask yourself: who benefits when you take 10 pills a day? Not you.
Arjun Seth
January 26, 2026 AT 16:56 PMYou think you’re being safe? You’re not. You’re just following instructions like a sheep. Who told you to take these pills? A doctor who saw you for 5 minutes. Who told you to keep this list? A nurse who doesn’t even know your name. The system is designed to keep you passive. Wake up. Question everything. Stop trusting the white coat.
Frank Geurts
January 28, 2026 AT 03:15 AMIt is imperative, and indeed non-negotiable, that individuals managing chronic conditions engage in rigorous, disciplined adherence to the Seven Rights of Medication Safety, as delineated in this exemplary exposition. Furthermore, it is incumbent upon the patient to maintain, in triplicate, a contemporaneously updated pharmaceutical inventory, which must be physically carried, digitally archived, and verbally confirmed at every clinical encounter. Failure to comply constitutes a dereliction of personal responsibility with potentially fatal consequences.
RUTH DE OLIVEIRA ALVES
January 30, 2026 AT 01:20 AMI’ve worked in primary care for 22 years. The most common cause of medication errors? Incomplete lists. Patients forget the aspirin. They don’t mention the turmeric capsules. They don’t realize that the ‘herbal tea’ their aunt gave them contains licorice root-which raises blood pressure. We’ve had patients end up in ICU because we didn’t know about the supplement. This isn’t paranoia. It’s clinical reality.
Jami Reynolds
January 31, 2026 AT 11:25 AMDid you know that the FDA allows drug interactions to go untested if the combination is ‘off-label’? That means your doctor could be prescribing you a cocktail of meds that have never been studied together. The system is rigged. They don’t test for interactions because it’s too expensive. Your ‘safe’ meds? They’re a gamble. You’re a lab rat.
Mike Berrange
February 2, 2026 AT 05:05 AMWho the hell wrote this? It’s like a corporate brochure for CVS. ‘Use a pill organizer!’ Wow, revolutionary. Meanwhile, people can’t afford the meds in the first place. You think a reminder app fixes $200 insulin copays? You think a list fixes the fact that your doctor won’t talk to your pharmacist? This is tone-deaf. It’s victim-blaming wrapped in a bow.
Annie Choi
February 3, 2026 AT 16:18 PMJust had my MUR at the pharmacy. Pharmacist flagged a CYP3A4 interaction between my statin and my grapefruit juice. I thought it was just ‘a little juice.’ Turns out it’s a pharmacokinetic nightmare. She adjusted my dose and gave me a free pillbox. That’s the kind of care we need more of. Not just docs-pharmacists as frontline safety nets.