Hydrochlorothiazide vs Alternatives: Drug Selector
Drug Comparison Summary
Hydrochlorothiazide
Thiazide Diuretic
Half-life: 6–15 hours
Risk: Low potassium
Chlortalidone
Thiazide-like Diuretic
Half-life: 40–60 hours
Benefit: Better for resistant HTN
Indapamide
Thiazide-like Diuretic
Half-life: 12–24 hours
Benefit: Good for elderly
Furosemide
Loop Diuretic
Half-life: 2–4 hours
Risk: Significant electrolyte loss
Spironolactone
Potassium-Sparing Diuretic
Half-life: 1.5–2 hours
Benefit: Prevents potassium loss
Lisinopril
ACE Inhibitor
Half-life: 12–24 hours
Benefit: No diuretic side effects
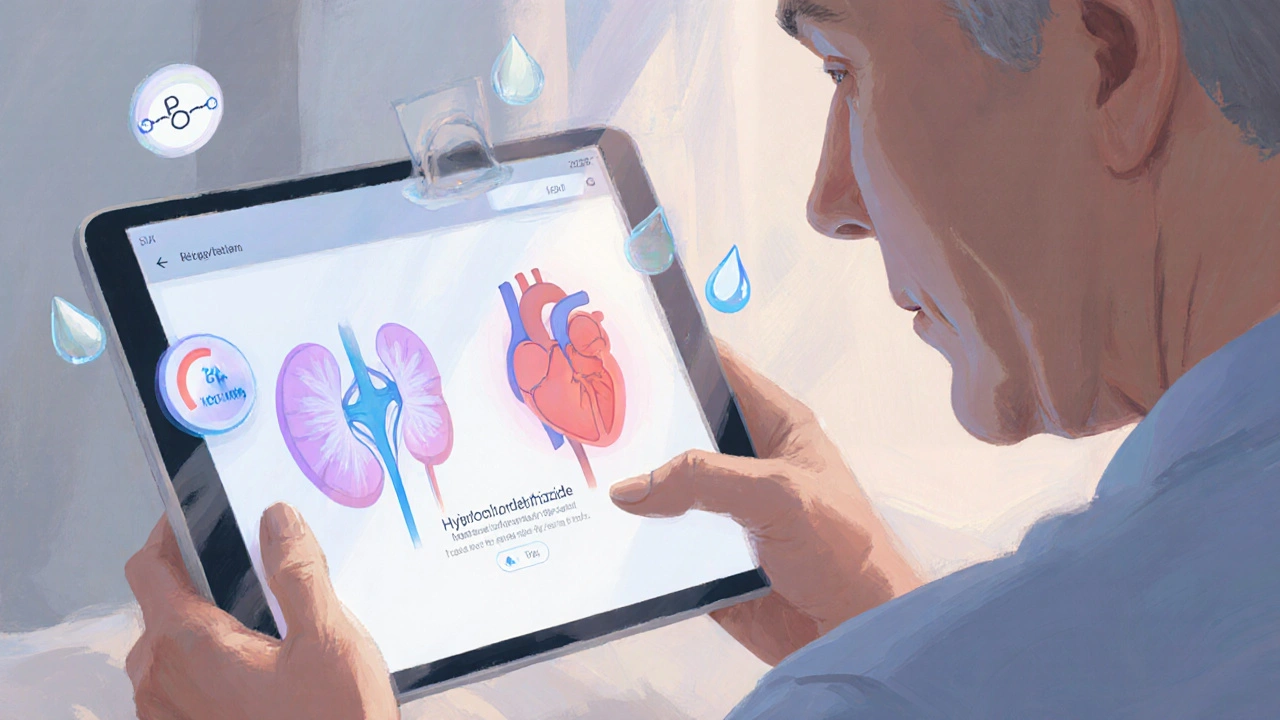
If you’ve been prescribed Hydrochlorothiazide and wonder how it stacks up against other blood‑pressure pills, you’re in the right place. This guide walks through the key facts, the pros and cons, and when you might consider a different option.
Key Takeaways
- Hydrochlorothiazide (HCTZ) is a first‑line thiazide diuretic for hypertension and mild edema.
- Chlortalidone and indapamide have longer half‑lives and often provide better blood‑pressure control.
- Loop diuretics like furosemide work faster but are usually reserved for more severe fluid overload.
- Potassium‑sparing agents such as spironolactone can counteract HCTZ‑induced potassium loss.
- Choosing the right drug hinges on kidney function, electrolyte profile, cost, and how your doctor tailors therapy.
What Is Hydrochlorothiazide?
Hydrochlorothiazide is a thiazide‑type diuretic that helps the kidneys eliminate excess sodium and water, lowering blood volume and thus blood pressure. First approved in the 1960s, it quickly became a staple for treating hypertension because it’s cheap, once‑daily, and works well for most patients.
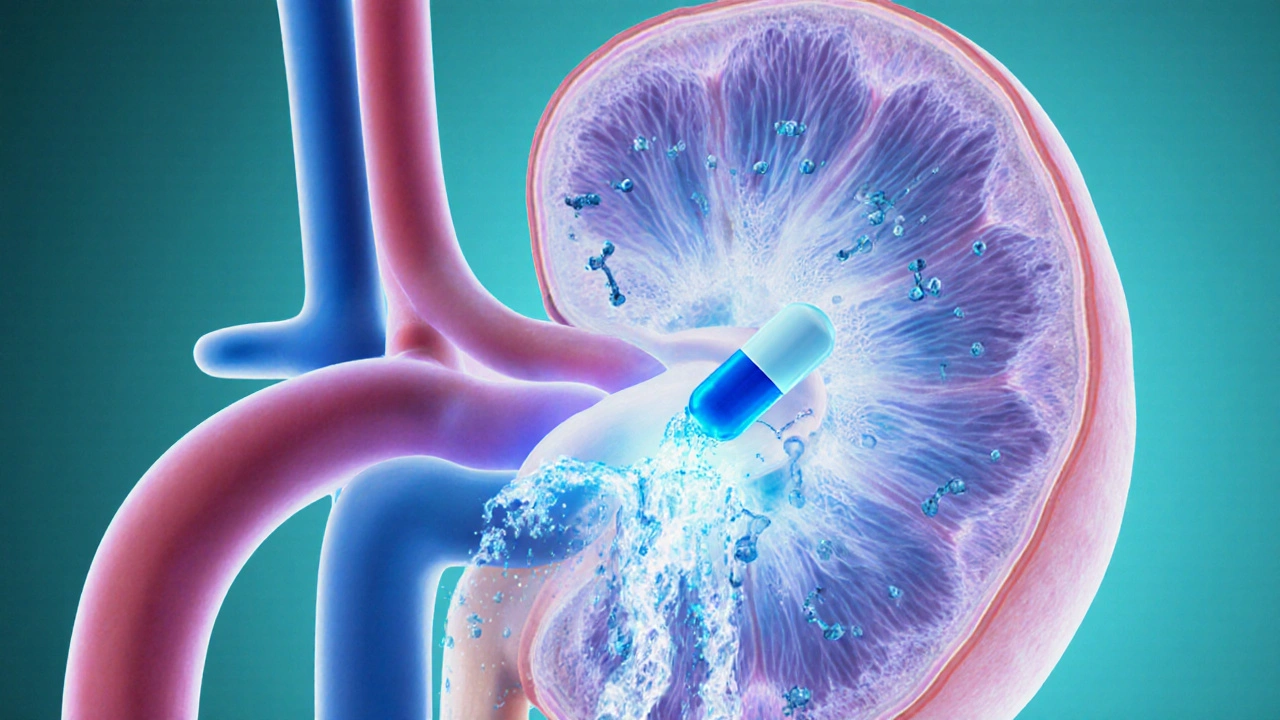
How Hydrochlorothiazide Works
The drug blocks the sodium‑chloride transporter in the distal convoluted tubule. By reducing sodium reabsorption, it pulls water into the urine, decreasing plasma volume. The modest drop in blood volume reduces cardiac output, and over time the vasculature relaxes, providing a lasting blood‑pressure drop.
Typical Dosing and Common Side Effects
Most adults start with 12.5mg to 25mg once daily, sometimes increased to 50mg if needed. The half‑life is about 6‑15hours, which is why a single dose covers a full day for many people. Common side effects include increased urination, mild dizziness, and electrolyte shifts-especially low potassium (hypokalemia) and a slight rise in uric acid that can trigger gout.

When Hydrochlorothiazide Falls Short
Even though HCTZ is effective for many, it isn’t perfect. Patients with chronic kidney disease (CKD) often need a drug that works longer in the renal tubules. Those who develop persistent low potassium may require a potassium‑sparing add‑on or a switch to another diuretic class.
Alternatives to Hydrochlorothiazide
Below are the most frequently considered alternatives, each with its own strengths.
Chlortalidone
Chlortalidone is a thiazide‑like diuretic with a longer half‑life (about 40‑60hours) and a stronger natriuretic effect. It’s often preferred for patients who need tighter blood‑pressure control or who have trouble adhering to multiple daily doses.
Indapamide
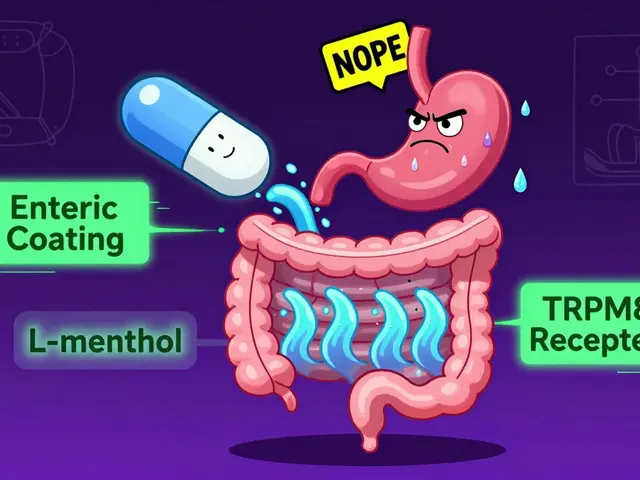
Indapamide combines thiazide activity with mild vasodilation. Its half‑life (12‑24hours) balances steady pressure reduction with a lower risk of electrolyte disturbance, making it a good fit for older adults.
Furosemide
Furosemide belongs to the loop diuretic class. It works upstream in the thick ascending limb, producing a rapid, powerful diuresis. While excellent for acute fluid overload (e.g., heart failure), it’s usually too aggressive for simple hypertension.
Spironolactone
Spironolactone is a potassium‑sparing diuretic that antagonizes aldosterone. It’s useful when HCTZ triggers low potassium or when resistant hypertension is present. It also helps with conditions like primary aldosteronism.
Lisinopril (ACE Inhibitor)
Lisinopril isn’t a diuretic but an ACE inhibitor that relaxes blood vessels directly. For patients who can’t tolerate thiazides due to gout or severe electrolyte issues, an ACE inhibitor offers a different pathway to lower pressure.
Side‑Effect Profiles Compared
All these drugs affect electrolytes, kidney function, and sometimes blood sugar. Here’s a quick snapshot:
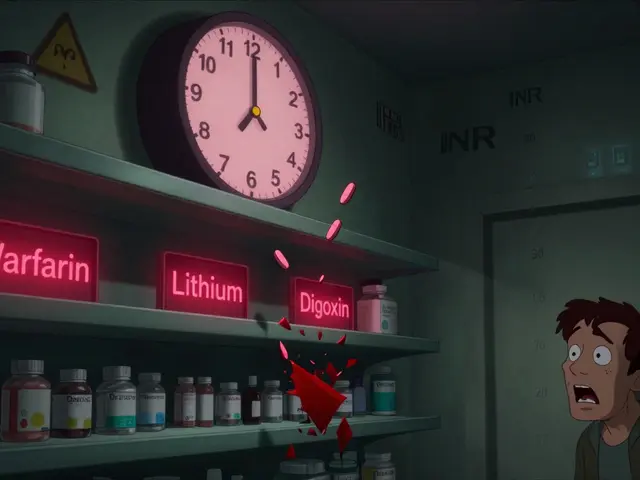
- Hydrochlorothiazide: Low potassium, modest uric acid rise.
- Chlortalidone: Similar electrolyte changes but often more pronounced due to longer action.
- Indapamide: Lower potassium loss; may cause mild headache.
- Furosemide: Can cause significant potassium and magnesium loss, dehydration.
- Spironolactone: Tends to raise potassium; may cause breast tenderness.
- Lisinopril: Cough, rare angioedema, can increase potassium.
Cost and Availability (2025 UK Context)
In the UK, generic HCTZ is the cheapest option, often below £1 per month on the NHS. Chlortalidone and indapamide are also generic and similarly priced. Furosemide is cheap but may require more frequent dosing. Spironolactone and lisinopril are modestly more expensive, though still covered by most prescriptions.
Side‑by‑Side Comparison Table
| Drug | Class | Typical Dose | Half‑Life | Effect on Potassium | Best Use Case | Typical Cost (UK, 2025) |
|---|---|---|---|---|---|---|
| Hydrochlorothiazide | Thiazide diuretic | 12.5‑50mg daily | 6‑15h | ↓ (hypokalemia) | First‑line hypertension | ~£1/month |
| Chlortalidone | Thiazide‑like diuretic | 12.5‑25mg daily | 40‑60h | ↓ (more pronounced) | Resistant hypertension | ~£1.20/month |
| Indapamide | Thiazide‑like diuretic | 1.5mg daily | 12‑24h | ↓ (mild) | Hypertension in older adults | ~£1.30/month |
| Furosemide | Loop diuretic | 20‑80mg daily | 2‑4h | ↓↓ (significant loss) | Acute fluid overload | ~£0.80/month |
| Spironolactone | Potassium‑sparing diuretic | 25‑100mg daily | 1.5‑2h | ↑ (hyperkalemia risk) | Resistant hypertension, aldosteronism | ~£2/month |
| Lisinopril | ACE inhibitor | 5‑40mg daily | 12‑24h | ↑ (possible hyperkalemia) | Patients intolerant to diuretics | ~£2.50/month |
How to Choose the Right Medication
Think of the decision like picking a tool for a specific job. Ask yourself these questions:
- Do you have any kidney issues? If eGFR < 30ml/min, a loop diuretic or an ACE inhibitor might be safer.
- Is low potassium a concern? If you’ve had cramps or arrhythmias, consider a potassium‑sparing agent or a lower‑dose thiazide‑like drug.
- Are you prone to gout? Thiazides can raise uric acid, so a non‑thiazide alternative (e.g., lisinopril) may be better.
- What’s your budget? Generic HCTZ remains the cheapest, but the NHS often covers all listed alternatives.
- How strict is your dosing schedule? Longer‑acting drugs (chlortalidone, indapamide) reduce the chance of missed doses.
Talk these points over with your GP or cardiologist. They’ll run blood tests (creatinine, electrolytes, uric acid) to see which drug matches your lab profile.
Real‑World Scenarios
Case 1 - Young professional with mild hypertension: Starts on 12.5mg HCTZ, tolerates it well, and blood pressure drops to 128/78mmHg. No side effects, cheap, perfect fit.
Case 2 - 68‑year‑old with CKD stage 3: HCTZ caused a mild rise in potassium and didn’t lower pressure enough. Doctor switches to indapamide 1.5mg daily; potassium stays stable, and BP reaches 132/80mmHg.
Case 3 - Patient with recurrent gout attacks: HCTZ worsened gout. Switching to lisinopril controlled blood pressure and eliminated gout flares.
Tips to Maximize Benefits & Minimize Risks
- Take your diuretic in the morning to avoid nighttime bathroom trips.
- Pair HCTZ with a low‑salt diet; the drug works best when you limit sodium.
- Check potassium levels after the first month; supplement if needed.
- If you feel dizzy, stand up slowly - the drop in blood volume can cause orthostatic hypotension.
- Never stop a diuretic abruptly without medical advice; the body can retain fluid quickly.
Frequently Asked Questions
Can I take Hydrochlorothiazide and an ACE inhibitor together?
Yes, many doctors combine a thiazide diuretic with an ACE inhibitor for synergistic blood‑pressure control. The ACE inhibitor can offset the potassium loss caused by HCTZ, but you’ll still need periodic electrolyte checks.
Why might my doctor switch me from Hydrochlorothiazide to Chlortalidone?
Chlortalidone has a longer half‑life, giving steadier blood‑pressure control, especially in people who miss doses or have resistant hypertension. It can also lower systolic pressure more effectively in some studies.
Is Hydrochlorothiazide safe during pregnancy?
It’s generally classified as Category B, meaning animal studies show no risk, but human data are limited. Most obstetricians prefer labetalol or methyldopa for hypertension in pregnancy.
What should I do if I develop gout while on Hydrochlorothiazide?
Talk to your GP about switching to a non‑thiazide option, such as an ACE inhibitor or calcium‑channel blocker. Meanwhile, lifestyle changes (low‑purine diet, hydration) and possibly a urate‑lowering drug can help.
How long does it take to see blood‑pressure improvement after starting Hydrochlorothiazide?
Most patients notice a drop within 1‑2 weeks, with the full effect by 4‑6 weeks. If you’re not seeing a change, your doctor may adjust the dose or add another medication.



Comments
OKORIE JOSEPH
October 6, 2025 AT 14:52 PMStop reading the pharma brochure and get real HCTZ alone works for most folks if you don’t mess it up. If you have potassium issues, add a bit of salty food.
Lucy Pittendreigh
October 14, 2025 AT 21:32 PMPeople who chase cheap pills ignore the bigger picture of health.
Nikita Warner
October 23, 2025 AT 04:12 AMHydrochlorothiazide remains a cornerstone in the management of uncomplicated hypertension due to its efficacy, safety profile, and low cost.
Its mechanism of action involves inhibition of the Na‑Cl cotransporter in the distal convoluted tubule, resulting in natriuresis and a modest reduction in plasma volume.
Clinical trials have demonstrated a mean systolic blood pressure reduction of 8–10 mmHg when used as monotherapy.
However, clinicians must remain vigilant for electrolyte disturbances, particularly hypokalemia and hyponatremia.
Routine monitoring of serum potassium at baseline and after dose adjustments is recommended to mitigate these risks.
In patients with concomitant gout, the uric acid‑raising effect of thiazides may precipitate attacks, warranting consideration of alternative agents.
When resistance to therapy emerges, switching to a thiazide‑like diuretic such as chlortalidone, which possesses a longer half‑life, often restores control.
Indapamide offers a similar antihypertensive potency with a more favorable potassium profile, making it suitable for elderly patients.
The choice between these agents should also reflect renal function; in chronic kidney disease stages 3–4, loop diuretics may be preferred for volume management.
Combination therapy with an ACE inhibitor or ARB can provide synergistic blood pressure lowering and offset potassium loss.
Cost considerations remain paramount in many health systems, and generic Hydrochlorothiazide typically costs less than £1 per month in the UK.
Nonetheless, the marginal price difference between thiazide‑like agents does not outweigh the clinical benefits in resistant cases.
Patients should be counseled to take the medication in the morning to avoid nocturnal diuresis.
A low‑sodium diet enhances the diuretic effect and reduces the need for dose escalation.
Finally, adherence is improved when dosing is once daily, reinforcing the importance of patient education in treatment success.
Liam Mahoney
October 31, 2025 AT 09:52 AMYo man HCTZ is not the be all and end all it can cause low potassium which i have seen many times.
surender kumar
November 8, 2025 AT 16:32 PMSure, because the cheapest drug is always the smartest choice, right.
Justin Ornellas
November 16, 2025 AT 23:12 PMOne must first acknowledge the linguistic precision inherent within the pharmacological nomenclature presented herein.
JOJO Yang
November 25, 2025 AT 05:52 AMGreat info.
Faith Leach
December 3, 2025 AT 12:32 PMThe pharma industry hides the truth about HCTZ side effects while pushing it as a miracle cheap fix.
Eric Appiah Tano
December 11, 2025 AT 19:12 PMRemember that informed decisions empower you and your doctor to choose the safest path together.
Jonathan Lindsey
December 20, 2025 AT 01:52 AMWhile the data may seem daunting, rest assured you will master your blood pressure with a sprinkle of patience and a dash of humor.
Gary Giang
December 28, 2025 AT 08:32 AMIndeed, pairing proper diet with the chosen diuretic often yields better outcomes than medication alone.
steve wowiling
January 5, 2026 AT 15:12 PMLife is but a fleeting echo of sodium and water dancing in our veins, and HCTZ is the conductor?
Warren Workman
January 13, 2026 AT 21:52 PMActually the metaphor fails; the renal tubule operates on osmotic gradients, not poetic whims.
Kate Babasa
January 22, 2026 AT 04:32 AMIt’s essential, therefore, to weigh both efficacy and safety, wouldn’t you agree?
Adam Martin
January 30, 2026 AT 11:12 AMAbsolutely, because while we contemplate the grand tapestry of antihypertensive stewardship, we must also remember the humble price tag that keeps patients from bankruptcy, a nuance often lost in clinical trials.
Ryan Torres
February 7, 2026 AT 17:52 PMWake up! The hidden agenda behind cheap diuretics is real 😡
shashi Shekhar
February 16, 2026 AT 00:32 AMYeah, sure, because the government is definitely plotting your potassium levels.