Blood Pressure Risk Assessment Tool
Risk Categories
- High Risk Systolic ≥140 mmHg or Diastolic ≥90 mmHg with multiple risk factors
- Moderate Risk Systolic 130-139 mmHg or Diastolic 80-89 mmHg with some risk factors
- Low Risk Normal blood pressure with minimal risk factors
When doctors talk about High Blood Pressure a chronic condition where the force of blood against artery walls stays elevated above normal levels, they’re warning about a silent attacker that chips away at the body's plumbing. Over time, this pressure overload can turn healthy vessels into stiff, leaky pipes, setting the stage for a cascade of serious illnesses. Managing high blood pressure early can keep your circulatory system running smooth and reduce the chance of life‑threatening events.
Why Blood Vessels Take a Hit
Every artery, vein, and capillary is lined with an endothelium a thin layer of cells that regulates vessel tone, blood clotting, and inflammation. Elevated pressure forces these cells to stretch, causing:
- Mechanical injury that triggers inflammatory pathways.
- Reduced nitric oxide production, leading to endothelial dysfunction the loss of the vessels' ability to relax and dilate properly.
- Accumulation of collagen and calcium, which makes arteries stiffer less elastic and more prone to damage.
Think of a garden hose left on full blast-it eventually cracks, leaks, and loses its ability to deliver water efficiently. The same physics applies inside your body.
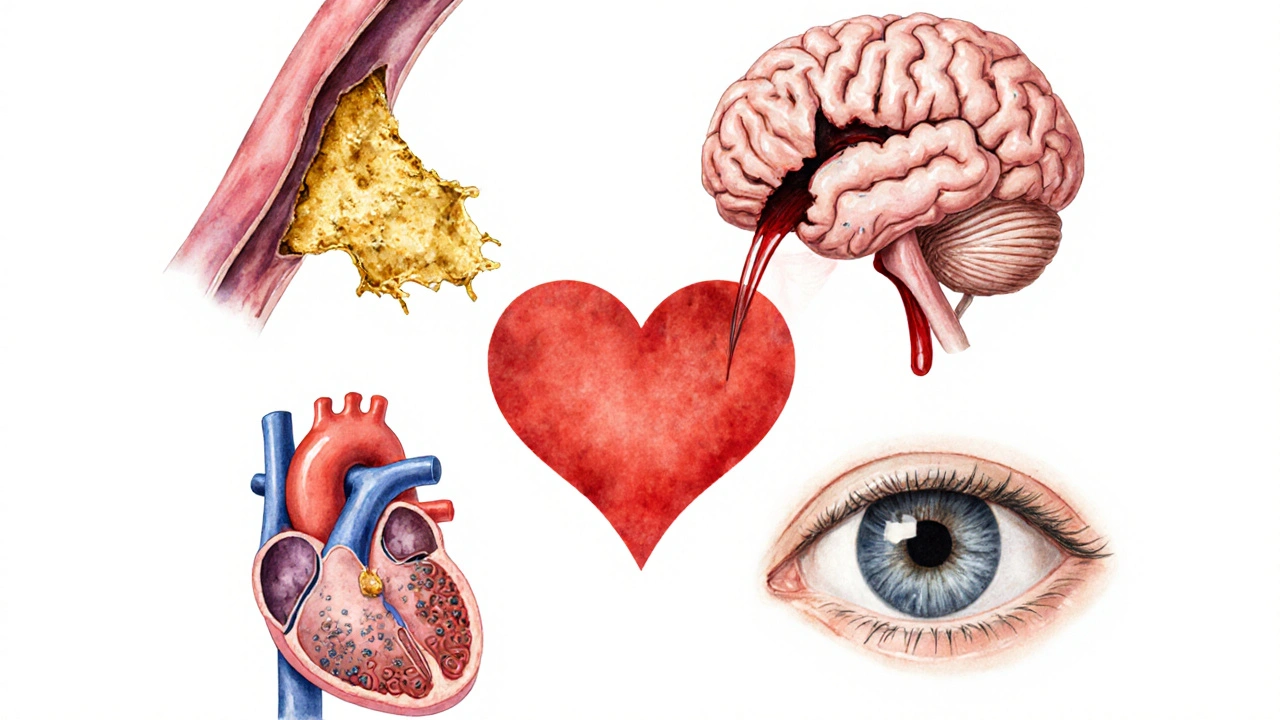
Major Diseases Linked to Hypertension
Atherosclerosis and Coronary Artery Disease
Chronic pressure accelerates the buildup of atherosclerotic plaques fatty deposits that narrow and harden arteries. Once plaques obstruct coronary arteries, the heart muscle receives less oxygen, raising the risk of a heart attack.
Stroke
High pressure can cause two types of stroke:
- Ischemic stroke - a clot forms in a narrowed artery, cutting off blood flow to the brain.
- Hemorrhagic stroke - a weakened vessel bursts, spilling blood into brain tissue.
Both scenarios lead to rapid brain cell death and long‑term disability. Studies from 2023 show that hypertension accounts for roughly 55% of all first‑time strokes worldwide.
Heart Failure and Myocardial Infarction
When the heart works against high resistance, it thickens (left‑ventricular hypertrophy) and eventually weakens. This progression can end in heart failure or a sudden myocardial infarction commonly known as a heart attack.
Kidney Disease
The kidneys filter blood through tiny vessels called glomeruli. Persistent high pressure damages these filters, leading to chronic kidney disease (CKD). About 30% of adults with stage 3 CKD also have hypertension, creating a vicious feedback loop.
Vision Problems
Retinal arteries are especially sensitive. Hypertensive retinopathy can cause micro‑aneurysms, bleeding, and even vision loss. Early eye exams can spot these changes before symptoms appear.
Risk Modifiers: Who’s Most Vulnerable?
Not everyone with a systolic reading of 130mmHg will develop these complications, but several factors raise the odds:
- Genetics family history of hypertension or early cardiovascular disease.
- Lifestyle factors high‑salt diet, excessive alcohol, sedentary behavior, and chronic stress.
- Age - arterial walls naturally stiffen after 45, amplifying pressure effects.
- Metabolic conditions - obesity, type2 diabetes, and dyslipidaemia.
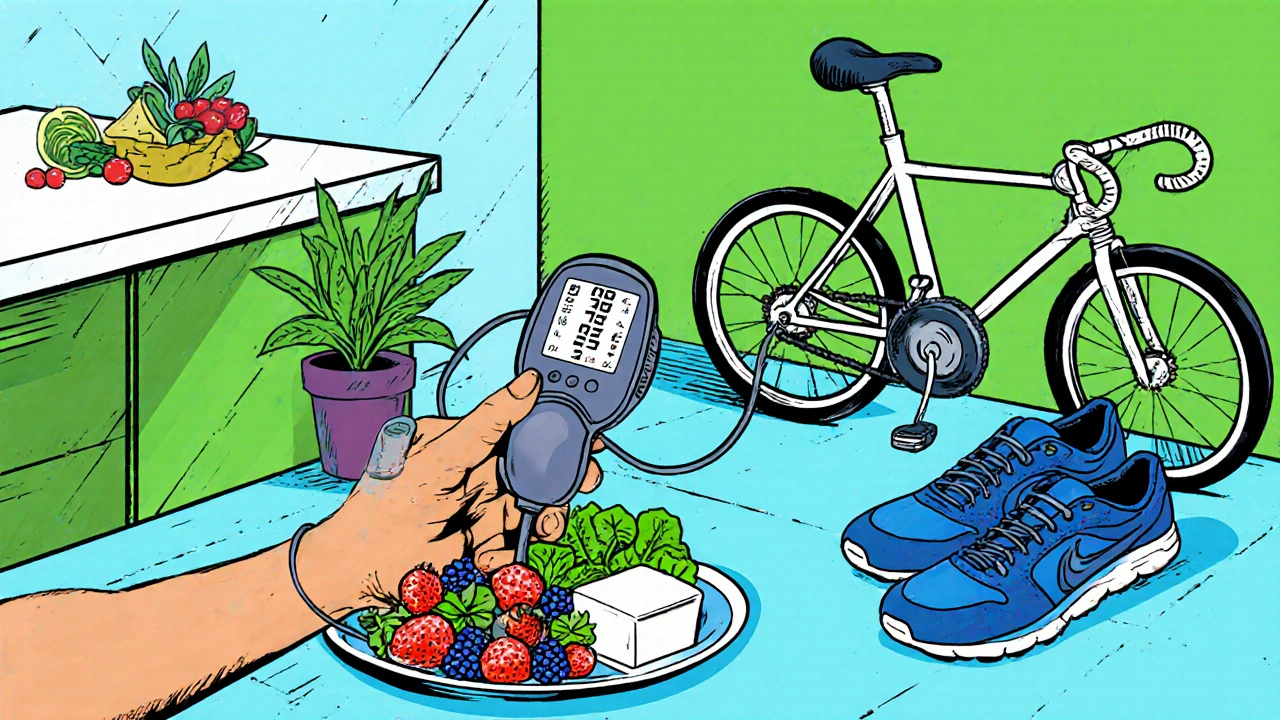
Prevention and Management Strategies
Knowing the damage path makes it easier to intervene. Here’s a practical roadmap:
- Monitor regularly. Home cuffs calibrated annually give a realistic picture of trends.
- Adopt the DASH diet. Aim for 1500‑2000mg of sodium daily, plenty of potassium‑rich fruits, and low‑fat dairy.
- Move daily. At least 150minutes of moderate aerobic activity (brisk walking, cycling) cuts systolic pressure by 5‑8mmHg on average.
- Limit alcohol. No more than two drinks per day for men, one for women.
- Stress management. Mindfulness, deep‑breathing, or short power‑naps can lower nighttime readings.
- Medication when needed. ACE inhibitors, ARBs, calcium‑channel blockers, or thiazide diuretics are first‑line choices, prescribed based on comorbidities.
Combine at least three lifestyle tweaks before relying on medication; many patients achieve target pressures (<120/80mmHg) without drugs.
Quick Checklist: Protect Your Vascular Health
- Check blood pressure at least once a week.
- Swap processed snacks for fresh fruit and nuts.
- Walk or jog 30minutes most days.
- Keep sodium < 2000mg per day.
- Schedule an eye exam every 2years.
- Review medication side‑effects with your GP annually.
Frequently Asked Questions
What blood pressure reading is considered high?
A systolic pressure of 130mmHg or higher, or a diastolic pressure of 80mmHg or higher, qualifies as hypertension according to the 2023 ACC/AHA guideline.
Can lifestyle changes reverse vascular damage?
Yes. Studies show that consistent diet, exercise, and weight loss can improve arterial elasticity and reduce plaque progression, especially when started early.
How does high blood pressure affect the kidneys?
Elevated pressure damages glomerular capillaries, decreasing filtration efficiency and eventually leading to chronic kidney disease. Controlling pressure slows this decline dramatically.
Is white‑coat hypertension real?
Yes. Some people experience a temporary spike in the doctor’s office due to anxiety. Home monitoring helps differentiate it from sustained hypertension.
What’s the link between hypertension and stroke?
High pressure weakens cerebral arteries, making them prone to blockages (ischemic stroke) or ruptures (hemorrhagic stroke). Managing pressure reduces stroke risk by up to 40%.





Comments
Alan Larkin
October 8, 2025 AT 14:18 PMNice try, but you’ve completely missed the point about sodium, mate 😊
John Chapman
October 9, 2025 AT 09:44 AMWhile the article offers a commendable overview, it neglects to address the nuanced interplay between renin‑angiotensin activation and vascular remodeling. The mechanistic cascade, as delineated in contemporary cardiology literature, extends far beyond simple pressure metrics. Moreover, the omission of ambulatory blood pressure monitoring undermines the practical applicability of the risk tool. A sophisticated reader will note that dietary sodium reduction alone fails to compensate for genetic predispositions. The author also glosses over the pivotal role of endothelial nitric oxide synthase dysregulation. In addition, recent meta‑analyses suggest that moderate alcohol consumption may exert a hormetic effect, a nuance absent from the discussion. Finally, the therapeutic algorithm would benefit from a stratified approach based on comorbid renal function. In short, the piece reads like a cursory public‑health pamphlet rather than an evidence‑based treatise.
Tiarna Mitchell-Heath
October 10, 2025 AT 05:11 AMSeriously? You’ve dressed up half‑truths in fancy jargon while ignoring the fact that most patients can’t even afford the suggested monitoring. Your elitist tone is as pointless as the missing data on socioeconomic factors.
Katie Jenkins
October 11, 2025 AT 00:38 AMFirst, the article correctly identifies hypertension as a silent threat, but it could improve clarity by distinguishing systolic from diastolic risks more explicitly. Second, the claim that “moderate alcohol may exert a hormetic effect” needs citation; otherwise it reads speculative. Third, the DASH diet recommendation is spot‑on, yet the sodium target of 1500‑2000 mg may be unrealistic for many cultural cuisines. Fourth, regular aerobic activity does indeed lower systolic pressure by 5‑8 mmHg, as shown in the 2022 ACC/AHA guideline. Finally, patients should be encouraged to use validated home monitors; the article’s brief mention of calibration is insufficient. Overall, a solid foundation that would benefit from tighter sourcing and practical guidance.
Jack Marsh
October 11, 2025 AT 20:04 PMWhile lifestyle modification is undeniably valuable, the implication that it can replace pharmacotherapy in moderate‑to‑high risk individuals is misleading. Numerous randomized controlled trials have demonstrated that, without antihypertensive agents, target blood pressures remain elusive despite diet and exercise alone. Furthermore, the article neglects to discuss potential drug–drug interactions in polypharmacy, a critical oversight for elderly patients. In short, a balanced approach integrating both non‑pharmacologic and pharmacologic strategies is essential.
Terry Lim
October 12, 2025 AT 15:31 PMSkip the sugar‑coated optimism; medication saves lives.
Cayla Orahood
October 13, 2025 AT 10:58 AMThe very air we breathe seems to conspire against our arteries when the pressure climbs unchecked.
Imagine a dam strained beyond its limits, each pulse a hammer striking steel, until the concrete cracks.
That crack is not a metaphor; it is the silent fissure appearing in the endothelium of every hypertensive soul.
Within minutes of that breach, inflammatory cascades flood the vessel walls like angry invaders.
Collagen and calcium deposit like villainous graffiti, turning supple tubes into rigid, unforgiving pipes.
The heart, forced to pump against this tyranny, bulks up its muscle in a desperate, maladaptive hypertrophy.
Yet the swollen muscle soon tires, and the once‑steady rhythm falters into a fatal arrhythmia.
Meanwhile, the kidneys, those diligent filters, are assaulted by the relentless pressure, their glomeruli scarred beyond repair.
A single episode of uncontrolled hypertension can precipitate an ischemic stroke that steals half a life in seconds.
And the brain, ever the fragile organ, endures hemorrhagic bursts that paint the skull with blood and terror.
Even the eyes are not spared; retinal vessels hemorrhage, leaving a veil of darkness where once clarity reigned.
The statistics are chilling: over half of all first‑time strokes worldwide bear hypertension as a culprit.
And yet, the pharmaceutical industry whispers sweet promises of pills while the public clings to the myth of “just eat less salt.”
The truth is far more brutal: without decisive intervention, each day adds inches to the canyon of risk.
It is not enough to “watch” your numbers; you must battle them with diet, movement, and, when needed, medicine.
In this war, complacency is the deadliest enemy, and awareness the only weapon we truly possess.
McKenna Baldock
October 14, 2025 AT 06:24 AMFrom a philosophical standpoint, the vascular system mirrors the delicate balance of mind and body; when pressure skews, equilibrium collapses. Your emphasis on endothelial health aligns with the principle of reciprocity in nature. Yet we must also acknowledge the societal structures that limit access to fresh produce and safe neighborhoods for exercise. By recognizing these external constraints, our solutions become more compassionate and effective. In essence, health is a shared ethical responsibility.
Roger Wing
October 15, 2025 AT 01:51 AMWell i guess hypertension is just a myth you know the stress is all mental
Matt Cress
October 15, 2025 AT 21:18 PMOh great another article telling us to drik water – as if we didn’t know that already.
Andy Williams
October 16, 2025 AT 16:44 PMThe article correctly states that “regular aerobic activity can lower systolic pressure by 5‑8 mmHg”, but it should use the singular “mmHg” rather than the plural “mmHg”. Additionally, the phrase “When the heart works against high resistance, it thickens (left‑ventricular hypertrophy) and eventually weakens” would be clearer as “When the heart works against high resistance, it undergoes left‑ventricular hypertrophy, which eventually leads to weakening.” Finally, the term “retinal arteries are especially sensitive” needs a comma after “especially”. These minor edits would enhance the piece’s precision.
Paige Crippen
October 17, 2025 AT 12:11 PMIt’s unsettling how quickly the narrative shifts from lifestyle advice to medication without acknowledging the hidden agenda of pharmaceutical lobbying. The subtle push for prescription drugs feels orchestrated, especially when the risk calculator downplays the role of genetics. One can’t help but wonder whose interests are truly being served.
sweta siddu
October 18, 2025 AT 07:38 AMHey everyone! 🌟 This post really breaks down how hypertension sneaks up on us. I love the tip about the DASH diet – swapping out salty snacks for fresh fruit makes a huge difference. Also, remember to stay active, even a quick 20‑minute walk can boost your mood and lower pressure. Keep sharing these gems! 😊
Ted Mann
October 19, 2025 AT 03:04 AMWe stand at the crossroads of knowledge and action; recognizing the science is only half the battle, the other half is willful implementation. Your suggestion to combine at least three lifestyle changes before medication mirrors the ancient wisdom of moderation. Yet, the modern world bombards us with convenience that erodes those very habits. Let’s champion community initiatives that make healthy choices the easy choices. Together, we can reshape the narrative from reactive treatment to proactive wellness.
Brennan Loveless
October 19, 2025 AT 22:31 PMPatriotic health isn’t just about personal responsibility; it’s about national strength. High blood pressure weakens the workforce, and a robust population is a strategic asset. While some claim that lifestyle tweaks are sufficient, data from the Department of Defense shows that comprehensive screening paired with timely pharmacotherapy saves both lives and tax dollars. Therefore, let’s adopt a policy that mandates regular blood pressure checks in all workplaces. Ignoring this is tantamount to compromising our collective security.
Vani Prasanth
October 20, 2025 AT 17:58 PMAbsolutely agree, Brennan. Implementing routine screenings is a practical step that respects both individual health and national interest. We can also provide educational workshops to demystify the hypertension risk tool, ensuring everyone feels empowered. Your suggestion aligns perfectly with a supportive, community‑focused approach.
Maggie Hewitt
October 21, 2025 AT 13:24 PMSure, let’s all drop everything and become hypertension vigilantes because a few extra minutes of walking will magically erase decades of arterial damage. In reality, incremental changes are the only realistic path, and they require patience, not dramatic proclamations. Still, kudos for the thorough breakdown – it’s a solid foundation for anyone looking to improve their cardiovascular health.
Mike Brindisi
October 22, 2025 AT 08:51 AMInteresting take but you really should have mentioned the importance of checking your cuff calibration regularly otherwise all those numbers are meaningless