GLP-1 Side Effect Tracker & Guidance Tool
Track Your Symptoms
Your Symptom Timeline
Personalized Guidance
Based on your symptom entry, nausea typically improves by [calculated date]
More than 1 in 8 Americans are now taking a GLP-1 receptor agonist-drugs like Ozempic, Wegovy, or Mounjaro-for diabetes or weight loss. These medications work wonders: they lower blood sugar, crush appetite, and help people lose up to 20% of their body weight. But for many, the price of success is a stomach that feels like it’s been turned inside out. Nausea, vomiting, bloating, and constipation aren’t just side effects-they’re the main reason people quit.
Why Do GLP-1 Drugs Make You Feel Sick?
It’s not a glitch. It’s the whole point.
GLP-1 agonists mimic a natural hormone that tells your body you’re full. One way it does this is by slowing down how fast your stomach empties. That’s great if you’re trying to eat less. But it also means food sits longer, gas builds up, and your gut feels backed up. The same mechanism that reduces hunger also triggers nausea. It’s not random. It’s biology.
Studies show between 40% and 85% of people on these drugs experience gastrointestinal side effects. Nausea hits hardest in the first few weeks, especially during dose increases. Liraglutide (Victoza) causes nausea in about 20-25% of users at full dose. Semaglutide (Ozempic, Wegovy) is a bit better-around 15-20%. But even those numbers don’t tell the full story. In real life, many people feel it worse than the trials suggest. Why? Because trials exclude people with sensitive stomachs or prior GI issues. Real patients aren’t that lucky.
When Does the Nausea Get Better?
The good news? It usually passes.
Most people report that nausea peaks during the first 4 to 6 weeks, especially while the dose is being ramped up. Once you hit the maintenance dose-usually after 16 to 20 weeks-the nausea starts to fade. A lot of users on Reddit’s r/Ozempic and r/Wegovy say the worst of it is over by week 8. Your body adapts. Your gut learns to work with the drug, not against it.
But here’s the catch: if you stop taking the drug because of nausea, you’ll never get to that point. That’s why doctors stress slow titration. Jumping straight to the full dose? Big mistake. Starting low and going slow gives your system time to adjust. Many patients who quit early could’ve stuck it out-if they’d known the nausea wasn’t permanent.
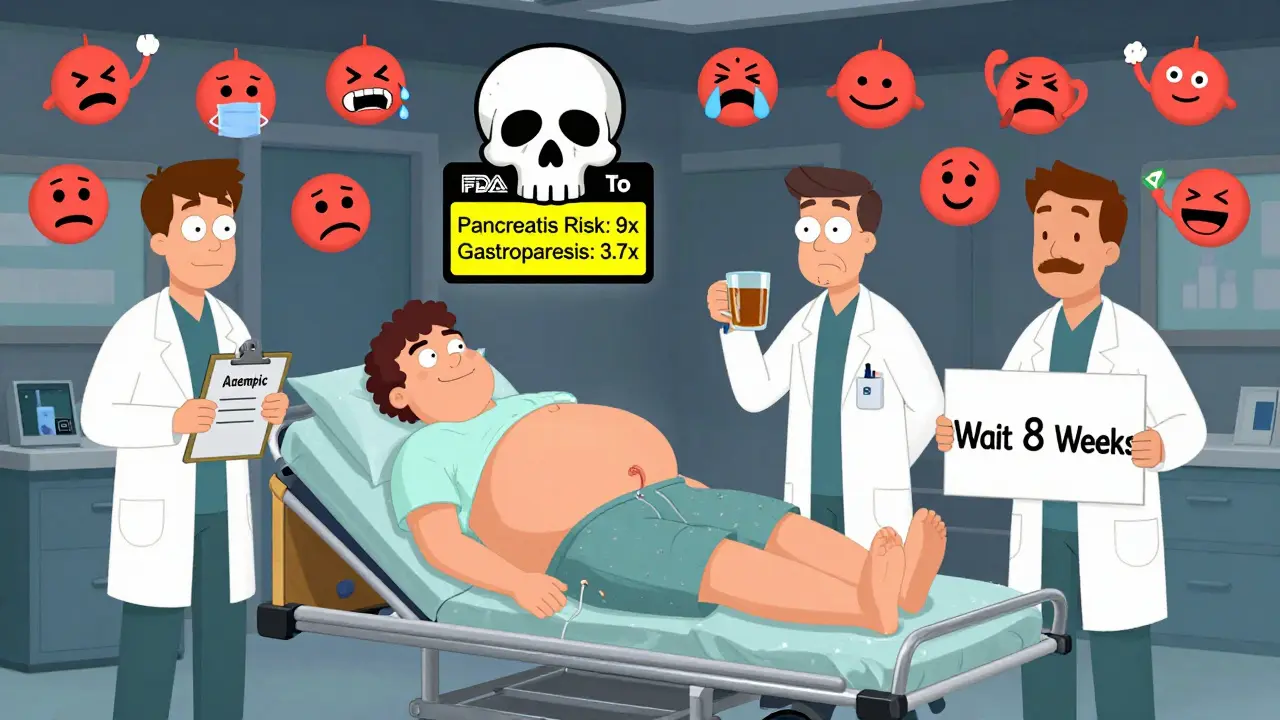
What Are the Real Risks Beyond Nausea?
Most GI side effects are uncomfortable, not dangerous. But some aren’t.
A 2023 JAMA study looked at over 5,000 people on GLP-1 drugs and found significantly higher risks of serious problems:
- Pancreatitis: 9 times more likely than with other weight-loss meds
- Bowel obstruction: 4 times more likely
- Gastroparesis (stomach paralysis): 3.7 times more likely
These are rare-but they’re real. If you’re vomiting nonstop, can’t pass gas or stool, or have sharp, constant pain in your abdomen, don’t wait. Go to the ER. Same if your skin or eyes turn yellow (jaundice) or you feel dizzy from dehydration.
There’s also a boxed warning-the FDA’s strongest-for thyroid tumors in animal studies. No proven cases in humans yet, but it’s something your doctor should discuss with you before you start.

How to Reduce Nausea Without Quitting
You don’t have to suffer through this. There are proven ways to make it bearable.
1. Eat Smaller, Simpler Meals
Large meals = more nausea. Fat and sugar make it worse. Stick to bland, low-fat foods: toast, rice, boiled potatoes, bananas, broth, plain yogurt. Avoid fried food, creamy sauces, pastries, and sugary drinks. Eat five small meals instead of three big ones. Chew slowly. Don’t rush.
2. Stay Hydrated, But Sip Slowly
Dehydration makes nausea worse. But chugging water can trigger vomiting. Sip small amounts throughout the day. Room temperature water is better than cold. Try herbal teas-ginger, peppermint, or chamomile. Ginger is especially helpful. Studies show it reduces nausea in pregnancy and chemotherapy patients. Why not here? Many users swear by ginger tea or ginger chews.
3. Don’t Lie Down After Eating
Gravity helps. Wait at least 2-3 hours after eating before lying down or going to bed. Sitting upright or walking lightly helps your stomach empty more easily.
4. Take It at Night
Some people find that taking their injection or pill before bed reduces nausea. Why? Because you’re asleep when the worst hits. You wake up, and the nausea is gone-or at least milder.
5. Talk to Your Doctor About OTC Help
Don’t self-medicate, but don’t suffer in silence either. Over-the-counter options like dimenhydrinate (Dramamine) or meclizine can help with nausea. Your doctor might also suggest anti-nausea meds like ondansetron, especially during the worst weeks. Always check with them first.
When to Stop-And When to Push Through
Not all nausea is the same.
If you’re mildly queasy after meals, have no appetite, and feel better after a few hours? That’s the common kind. Stick with it. Give it 6-8 weeks.
If you’re vomiting multiple times a day, can’t keep fluids down, have severe abdominal pain, or haven’t had a bowel movement in 3+ days? That’s not normal. Call your doctor. You might need to pause the drug, adjust the dose, or rule out something more serious like gastroparesis or ileus.
Remember: stopping the drug because of nausea doesn’t mean you failed. It means you didn’t have the right support. Many people who quit early could’ve succeeded with better guidance.
What’s Next? Better Drugs on the Horizon
Pharma companies know the side effects are holding back adoption. That’s why they’re racing to build better versions.
New GLP-1 drugs are being tested with slower-release formulations, oral delivery systems, and combo therapies that use lower doses of GLP-1 with other agents. The goal? Keep the weight loss and blood sugar control, but cut the nausea.
One drug already approved-tirzepatide (Mounjaro)-works on two hormones, not just one. Some users report less nausea than with semaglutide, though data is still emerging. Early signs suggest future versions will be easier on the gut.
The Bottom Line
GLP-1 receptor agonists are powerful tools. They’re changing how we treat obesity and diabetes. But they’re not magic pills. They’re powerful medicines with real, common, and often intense side effects.
If you’re on one, know this: nausea is not a sign you’re doing something wrong. It’s a sign your body is responding. Most people get through it. Many end up losing 15% or more of their body weight. But you need patience, the right diet, and a doctor who understands.
Don’t quit too soon. Don’t ignore warning signs. And don’t assume you have to suffer. There are ways to make this work-without giving up the results you want.



Comments
Charles Barry
December 24, 2025 AT 18:33 PMLet me guess-Big Pharma paid off the FDA to hide the fact that these drugs are just slow-acting poison with a fancy label. They slow your stomach so much your intestines start staging a coup. And don’t get me started on the thyroid tumor warning-why do you think they buried it in a ‘boxed warning’? Because they know people will ignore it until they’re lying in a hospital with a tumor the size of a grapefruit. This isn’t medicine. It’s a corporate experiment on the desperate.
Joe Jeter
December 26, 2025 AT 04:03 AMPeople act like nausea is the worst thing that could happen. Back in my day, we didn’t have fancy drugs-we had willpower. Eat less. Move more. No magic injections. Now everyone wants a pill that makes them thin without lifting a finger, and when it gives them a queasy stomach, they cry like it’s a crime. If you can’t handle a little discomfort for 8 weeks, maybe you shouldn’t be trying to lose weight at all.
Sidra Khan
December 27, 2025 AT 21:05 PMI took Ozempic for 3 months. Nausea hit hard week 2. I cried at lunch. But I stuck with it. By week 7, I could eat a burger without wanting to die. Lost 22 lbs. No regrets. Just don’t start at the max dose. And yes, ginger tea is magic. 🍵
Lu Jelonek
December 29, 2025 AT 04:09 AMAs someone who works in endocrinology, I see this daily. The real issue isn’t the nausea-it’s the lack of nutritional counseling. Patients get the script and zero guidance on how to eat. They eat pizza and expect not to feel sick. The drug isn’t the villain. The advice is. Pair this with a dietitian, not just a doctor. That’s the missing piece.
siddharth tiwari
December 31, 2025 AT 03:50 AMguyz its not just nausea… its the gmo corn syrup in the fillers that makes it worse. i read on a forum that the gel caps have glyphosate. thats why my stomach felt like it was being chewed by spiders. switched to generic and i feel better. also the gov is hiding the truth. they dont want you to know its all about profits.
Andrea Di Candia
January 2, 2026 AT 00:19 AMIt’s funny how we treat these drugs like they’re the enemy. They’re just molecules doing what they’re designed to do-signal fullness. The real problem is our culture of instant gratification. We want weight loss without discomfort, without change, without patience. Nausea isn’t a flaw in the drug-it’s a mirror. It’s showing us how out of sync we are with our own biology. Maybe the real medicine is learning to listen.
bharath vinay
January 2, 2026 AT 08:16 AMThey say it gets better after 8 weeks? LMAO. That’s what they told us about the vax. Now look at the long-term data-people are still puking after a year. And the pancreatitis risk? That’s not rare. It’s just not reported because the FDA lets pharma bury the bad stuff. You think they’d approve this if it was a natural herb? Nah. It’s a patentable chemical. That’s the only reason it’s on the market.
Dan Gaytan
January 4, 2026 AT 06:40 AMI was terrified to start this because I have IBS. But I followed the slow titration and the bland diet advice. Honestly? Week 4 was brutal, but by week 6, I could eat rice and chicken without panic. I didn’t lose 20%, but I lost 14% and my A1c dropped from 7.8 to 5.9. It’s not perfect, but it’s worth it. If you’re scared, start low. And drink ginger tea. It’s like a hug for your gut. 🤍
Usha Sundar
January 5, 2026 AT 21:40 PMMy mom took it. Vomited every day for 6 weeks. Quit. Said she’d rather be fat than feel like she’s dying. Fair.
Wilton Holliday
January 6, 2026 AT 07:39 AMTo everyone saying ‘just push through’-thank you for the advice, but not everyone can. Some of us have anxiety disorders, chronic nausea from past illnesses, or just can’t physically handle it. That doesn’t make us weak. It makes us human. The goal isn’t to force people into suffering-it’s to help them find a path that works. If GLP-1s aren’t it for you, there are other ways. You’re not failing. You’re choosing yourself. And that’s brave too.