When you’ve had a heart attack or a stent placed, your doctor gives you a blood thinner-not to thin your blood like water, but to stop platelets from clumping together and forming dangerous clots. Three drugs dominate this space: clopidogrel, prasugrel, and ticagrelor. They all block the same receptor on platelets, but their side effects? They’re not the same. And choosing the wrong one can mean the difference between staying out of the hospital and ending up in the ICU.
Why These Drugs Even Exist
Before these three, aspirin was the go-to. But for people with acute heart problems, aspirin alone isn’t enough. That’s where P2Y12 inhibitors come in. They block a specific signal that tells platelets to stick together. Clopidogrel came first in 1997, then prasugrel in 2009, and ticagrelor in 2011. Each one was designed to be stronger, faster, or more reliable than the last. But with more power comes more risk-especially when it comes to bleeding.These drugs are almost always taken with aspirin. That’s called dual antiplatelet therapy, or DAPT. It works great at preventing heart attacks and stent clots. But it also makes bleeding more likely. In fact, about 1 in 5 people on DAPT will have some kind of bleeding problem within a year. Not all of them are serious, but some can be life-threatening.
The Bleeding Risk: Who’s Most at Risk?
Bleeding is the biggest side effect across all three drugs. But not all bleeding is equal-and not all patients face the same risk.Prasugrel has the highest bleeding rate. In the TRITON-TIMI 38 trial, patients on prasugrel had 2.4% major bleeding compared to 1.8% on clopidogrel. That might sound small, but it’s a 33% increase. And fatal bleeding? Twice as high. That’s why prasugrel comes with a black box warning from the FDA: don’t use it if you’ve had a stroke or TIA, or if you’re over 75. In elderly patients, the risk skyrockets. One cardiologist I spoke with said, “I’ve seen too many fragile 80-year-olds with hemoglobin drops from 12 to 8 g/dL on prasugrel.”
Ticagrelor isn’t far behind. In the PLATO trial, it increased non-CABG major bleeding to 2.6% versus 2.3% for clopidogrel. That’s a small difference, but it’s consistent-and it adds up over time. Intracranial bleeding, the most dangerous kind, happens in about 0.1-0.3% of patients on any of these drugs. It’s rare, but when it happens, it’s often fatal.
Clopidogrel has the lowest bleeding risk of the three. But here’s the catch: it doesn’t work for everyone.
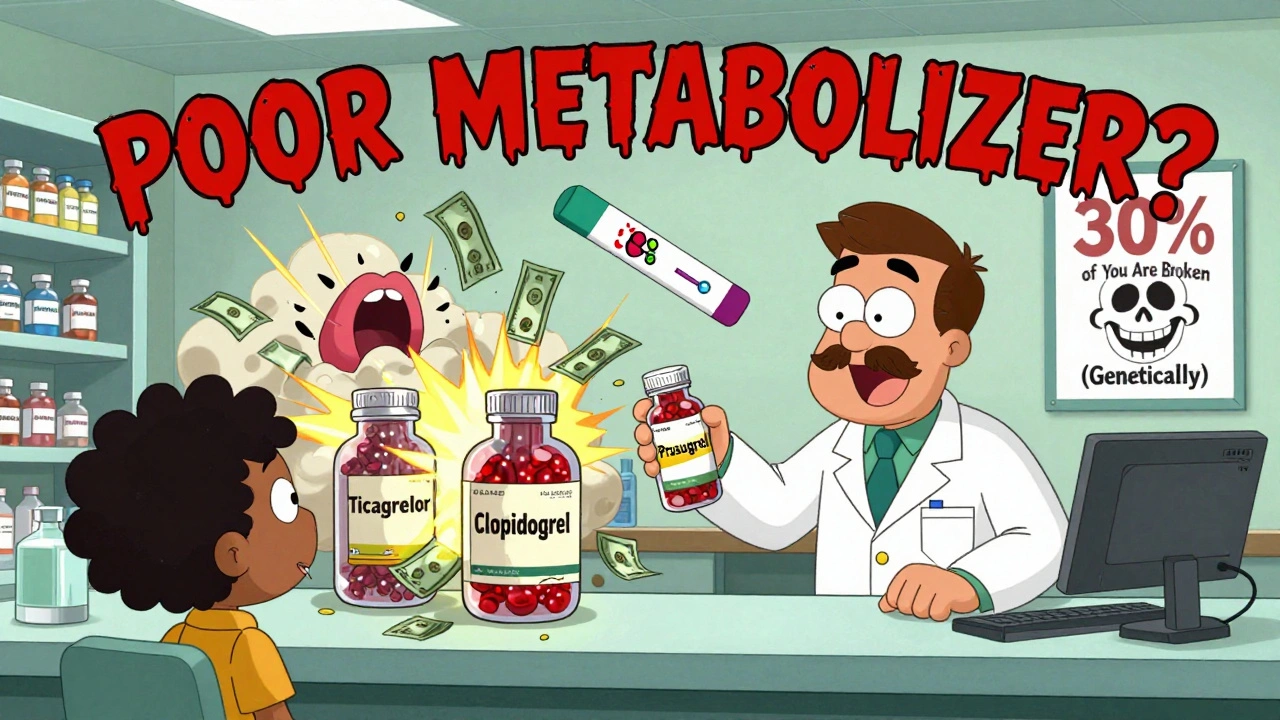
Clopidogrel’s Hidden Flaw: The “Poor Metabolizer” Problem
Clopidogrel isn’t active when you swallow it. Your liver has to convert it into the real thing using an enzyme called CYP2C19. About 30% of people-especially those of Asian descent-have a genetic variation that makes this enzyme weak or broken. These people are called “poor metabolizers.” For them, clopidogrel might as well be sugar pills.Studies show that poor metabolizers have a 3-5 times higher risk of stent clots or another heart attack. That’s not theoretical. I’ve seen patients who had a stent, took clopidogrel for months, then had a second heart attack. Their blood tests showed no platelet inhibition. They weren’t noncompliant. They just didn’t metabolize the drug.
Genetic testing for CYP2C19 exists. It costs $200-$300. But guidelines don’t recommend it for everyone. Why? Because it’s not cost-effective for the average patient. But if you’re young, have diabetes, or had a bad heart attack, it’s worth asking about.
Ticagrelor’s Weird Side Effect: Can’t Breathe
Ticagrelor is the only one of the three that doesn’t need liver conversion. It works directly. That means more consistent effects. But it comes with a strange, under-discussed side effect: trouble breathing.In the PLATO trial, 14-16% of people on ticagrelor said they felt short of breath. That’s compared to 8-10% on placebo. It’s not asthma. It’s not heart failure. It’s just… a feeling like you can’t get enough air. Some patients describe it as “feeling like I’m drowning.” It usually starts within days of starting the drug. It’s not dangerous in most cases-your oxygen levels are fine-but it’s terrifying.
And here’s the kicker: 15-20% of people who experience this stop taking ticagrelor. That’s a big problem. If you stop, your risk of clotting goes up fast. The good news? If you’re warned ahead of time, 60-70% of people stick with it. Your doctor should say, “You might feel short of breath. It’s not your heart. It’s the drug. It usually gets better in a few weeks.” That simple conversation keeps people alive.
Ticagrelor also causes brief pauses in your heartbeat-ventricular pauses. About 3% of people get them. They’re usually harmless, but if you have a pacemaker or a history of slow heart rhythms, your doctor needs to know.
Prasugrel: Powerful, But Only for the Right Patients
Prasugrel is the strongest platelet blocker. It works faster and more completely than clopidogrel. For patients with high-risk blockages, especially those getting a stent during a heart attack, it saves lives.But it’s not for everyone. The TRITON-TIMI 38 trial showed that for patients over 75, the bleeding risk jumps to 2.7%. For those under 60 kg (about 130 lbs), it’s 2.7% versus 1.7% on clopidogrel. That’s why doctors avoid it in older, smaller patients. Even if they’re otherwise healthy.
And if you need surgery? Prasugrel sticks around longer. You need to stop it 7 days before non-emergency surgery. Clopidogrel? 5 days. Ticagrelor? Just 3. That matters if you’re scheduled for a hip replacement or colonoscopy. Waiting longer means more clot risk. Stopping sooner means more bleeding risk. It’s a tightrope walk.

Cost, Convenience, and Real-World Choices
Let’s talk about money. Clopidogrel is a generic. It costs about $10 a month. Ticagrelor and prasugrel? Around $300-$400 a month. Insurance often covers them, but not always. And if you’re paying out of pocket? That’s a deal-breaker for many.Dosing matters too. Clopidogrel and prasugrel are once daily. Ticagrelor? Twice daily. That’s harder to remember. Miss a dose? Your platelets start waking up. That’s why adherence is lower with ticagrelor. One 2018 study found 21% more people quit ticagrelor because of side effects than clopidogrel.
Cardiologists have clear preferences. A 2022 poll of over 1,200 doctors showed 42% pick ticagrelor for most ACS patients because it’s reliable. 35% stick with clopidogrel because it’s cheap and familiar. Only 23% use prasugrel-and mostly for young, high-risk patients with no history of stroke or bleeding.
What’s New in 2025?
The landscape is shifting. In 2023, the FDA approved a lower dose of ticagrelor: 60 mg twice daily, instead of 90 mg. The MATTERHORN trial showed this lower dose cuts bleeding by 25% while still preventing heart attacks. Now, guidelines recommend starting with 90 mg for the first year after a heart attack, then switching to 60 mg for long-term use.Also, doctors are getting better at personalizing treatment. If you’re young and healthy with a big clot, go with prasugrel or ticagrelor. If you’re older, smaller, or have a history of bleeding, clopidogrel might be safer-even if it’s less powerful. And if you’re on a tight budget? Clopidogrel is still the most common choice worldwide.
Future drugs are coming. Selatogrel, a new injectable P2Y12 inhibitor, is in phase 3 trials. It works in minutes and wears off in hours. Imagine being able to turn off your blood thinner before surgery-without waiting days. That could change everything.
Bottom Line: Which One Should You Be On?
There’s no single best drug. It depends on your age, weight, bleeding risk, genetics, and lifestyle.- If you’re under 75, healthy, and had a major heart attack with a stent? Prasugrel gives you the best protection-but only if you’re not at high bleeding risk.
- If you’re over 75, have diabetes, or need surgery soon? Ticagrelor is often the better pick. Just be ready for possible shortness of breath.
- If you’re cost-sensitive, older, or have a history of bleeding? Clopidogrel is still a solid choice. But ask your doctor if you’re a poor metabolizer.
And no matter which one you’re on-never stop without talking to your doctor. Stopping suddenly can trigger a heart attack. Even if you feel fine.
Which antiplatelet drug has the least bleeding risk?
Clopidogrel has the lowest bleeding risk among the three, but it’s not always the safest choice. While it causes fewer major bleeds than prasugrel or ticagrelor, it doesn’t work well in about 30% of people due to genetic differences. So while bleeding risk is lower, the risk of a clot may be higher in those patients. For most people, the trade-off is worth it, but your doctor should assess your personal risk factors before choosing.
Why does ticagrelor cause shortness of breath?
The exact reason isn’t fully understood, but ticagrelor blocks a receptor in the lungs called adenosine A2A. This receptor helps regulate breathing signals. When blocked, it can cause a sensation of breathlessness-even when oxygen levels are normal. It’s not dangerous for most people, but it’s very unsettling. About 1 in 7 patients experience it, and it usually improves over time. Telling patients this upfront reduces discontinuation rates by nearly half.
Can I switch from clopidogrel to ticagrelor if it’s not working?
Yes, and it’s often recommended if you’re a poor metabolizer of clopidogrel. If you’ve had a stent and then a second clot, or if platelet testing shows you’re not responding, switching to ticagrelor or prasugrel can cut your risk of another event by up to 40%. The switch is done under medical supervision-usually with a loading dose. Don’t switch on your own. Timing matters, and stopping clopidogrel too soon can increase clot risk.
How long should I take these drugs after a stent?
The standard is 6 to 12 months of dual therapy (aspirin + P2Y12 inhibitor) after a stent. For high-risk patients-like those with diabetes or multiple blockages-doctors may extend it to 12-36 months. After that, you usually stay on aspirin alone. In 2023, guidelines added an option: switch to low-dose ticagrelor (60 mg twice daily) for long-term use. This reduces bleeding risk while still protecting against clots. Your doctor will decide based on your balance of clotting and bleeding risks.
Is prasugrel safe for elderly patients?
Generally, no. Prasugrel is not recommended for patients over 75, especially if they weigh less than 60 kg. Studies show bleeding rates nearly double in this group. Even if they seem healthy, their blood vessels are more fragile, and their bodies clear the drug slower. Many cardiologists avoid prasugrel in patients over 70 entirely. If you’re elderly and need strong antiplatelet therapy, ticagrelor or clopidogrel are safer choices.
What should I do if I need surgery while on one of these drugs?
Tell your surgeon and cardiologist well in advance. You’ll need to stop the drug before surgery to reduce bleeding risk. Clopidogrel: stop 5 days before. Prasugrel: stop 7 days before. Ticagrelor: stop 3 days before. Never stop on your own. If your surgery is urgent, your team may use bridging strategies or reverse the effect with platelet transfusions. But timing matters-stopping too early increases clot risk; stopping too late increases bleeding risk. Always coordinate care between your heart doctor and surgeon.





Comments
Irving Steinberg
December 2, 2025 AT 19:56 PMSo basically if you're old and cheap, you get the sugar pill that might not work but won't kill you. If you're young and dumb, you get the nuclear option that'll bleed you out. And if you're rich? Congrats, you get the one that makes you feel like you're drowning 🤯
Lydia Zhang
December 4, 2025 AT 15:59 PMTicagrelor breathing thing is real. I was on it for six months. Felt like a fish out of water. No idea why docs don't warn people better.
Kay Lam
December 5, 2025 AT 19:14 PMIt's important to remember that these drugs aren't one-size-fits-all and that individual biology plays a huge role in how they affect us. Some people have genetic variations that make clopidogrel ineffective, and that's not their fault. We need to move toward personalized medicine instead of just prescribing the most popular option because it's cheaper or easier. It's not just about bleeding risk or cost-it's about dignity and autonomy in healthcare decisions. Many patients aren't even told about genetic testing options, and that's a systemic failure.
Matt Dean
December 7, 2025 AT 10:30 AMAnyone who takes clopidogrel without getting tested for CYP2C19 is playing Russian roulette with their heart. You think you're saving money? You're just delaying the inevitable trip to the ER. And yes, I've seen it. Multiple times.
Walker Alvey
December 9, 2025 AT 06:16 AMSo we've turned medicine into a choose-your-own-adventure where the stakes are your life and the options are written by Big Pharma and insurance adjusters. How poetic
Adrian Barnes
December 10, 2025 AT 12:52 PMIt is imperative to underscore the statistical significance of the increased major bleeding events observed in the TRITON-TIMI 38 trial, particularly in elderly and low-weight populations. The hazard ratio for fatal hemorrhage with prasugrel versus clopidogrel is 2.1, with a 95% confidence interval of 1.4–3.2. This is not anecdotal; it is evidence-based medicine. Disregarding these parameters constitutes a breach of the standard of care.
Declan Flynn Fitness
December 11, 2025 AT 18:40 PMBig thanks for laying this out so clearly. I’ve been on ticagrelor for a year and the shortness of breath freaked me out at first-until my cardiologist said, ‘It’s the drug, not your heart.’ Now I know it’s just a weird side effect. Told my buddy who’s about to start it, and he’s way less scared now. 💪❤️
Michelle Smyth
December 12, 2025 AT 16:39 PMThe commodification of cardiac pharmacotherapy under neoliberal healthcare paradigms is profoundly dystopian. One cannot help but observe the epistemic violence inherent in reducing complex pharmacogenomic phenotypes to cost-benefit matrices dictated by formulary committees rather than molecular biology. Ticagrelor’s adenosine A2A antagonism, while clinically significant, is merely a symptom of a broader ontological crisis in cardiovascular therapeutics.
Patrick Smyth
December 12, 2025 AT 19:53 PMI had a stent last year. Took clopidogrel. Two months later, I had another heart attack. My doctor said I was a poor metabolizer. I didn't know that was even a thing. I almost died because no one told me. Now I'm on ticagrelor. I feel like I'm breathing underwater but I'm alive. Please, if you're on clopidogrel-ask for the test. Don't wait like I did.