More than 40 million Americans take statins to lower cholesterol and protect their hearts. But for a lot of people, the side effects make it hard to keep taking them. The most common problem? Muscle pain. It’s not just a minor annoyance-it’s one of the main reasons people stop statins, even when they need them. The good news? Most cases of muscle pain aren’t actually caused by the statin. And even if they are, there are effective alternatives that work.
What Is Statin Intolerance, Really?
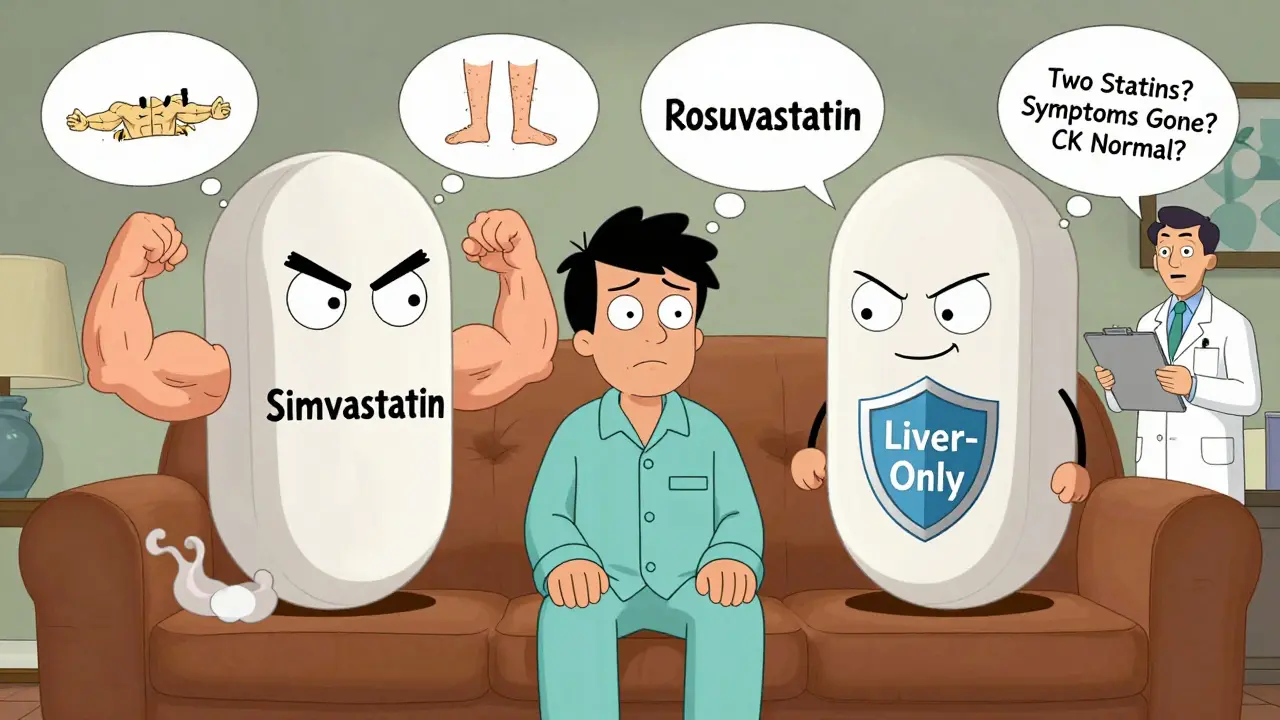
Statin intolerance isn’t just when you feel sore after starting a pill. According to the National Lipid Association (2022), it’s a specific diagnosis: you have to be unable to tolerate two different statins. One at the lowest dose, and another at any dose. And the symptoms must go away when you stop the drug. That’s it. No guesswork. No one-off reactions. Most people who think they’re intolerant aren’t. Studies show that up to 85% of patients who say they have statin-related muscle pain actually have the same symptoms when they take a placebo. That’s the nocebo effect-your brain expects side effects, so you feel them. This isn’t all in your head. It’s a real psychological response to fear, misinformation, or even a bad experience with a previous medication. True statin intolerance is rare. The actual risk of serious muscle damage from statins? About 5 in every 1,000 people per year. Compare that to the placebo group: 4.9 in 1,000. That’s almost the same. Most muscle symptoms are mild, temporary, and not dangerous. They don’t mean you’re at risk of rhabdomyolysis-a condition so rare, it affects fewer than 2 in a million statin users.What Do Statin Muscle Symptoms Actually Feel Like?
If you’re experiencing muscle issues, pay attention to where and how they show up. Statin-associated muscle symptoms (SAMS) usually hit the large muscles: thighs (78% of cases), buttocks (65%), back (52%), and shoulders (47%). It’s not sharp pain. It’s more like:- Heaviness-like your legs are filled with sand
- Stiffness-especially in the morning or after sitting
- Cranking or cramping-not constant, but annoying
- Weakness-struggling to get up from a chair or lift your arms
Why Do So Many People Stop Statins-And Why They Shouldn’t
About half of all statin prescriptions get stopped within the first year. Muscle pain is the top reason. But here’s the catch: people who stop statins without proper evaluation are at higher risk of heart attack, stroke, and death. One study found that inappropriate discontinuation increases cardiovascular events by 25%. That’s huge. The problem? Many doctors don’t follow the official guidelines. They hear “I feel sore,” and they stop the statin. But the right approach? First, confirm it’s really the statin. Then, try another statin. Then, consider alternatives. Studies show that 65% of people who can’t tolerate one statin can handle another. Why? Because not all statins are the same. Lipophilic statins like simvastatin and atorvastatin cross into muscle tissue more easily. That’s why they’re linked to more symptoms. Hydrophilic statins like pravastatin and rosuvastatin stay mostly in the liver. They’re gentler on muscles. Try this: if you stopped simvastatin because of leg pain, switch to rosuvastatin at 5mg. It’s just as effective at lowering LDL, but with 28% fewer muscle complaints. And if 10mg of atorvastatin caused trouble, try 5mg. You still get 32% LDL reduction-with 89% tolerability.What If You Really Can’t Tolerate Any Statin?
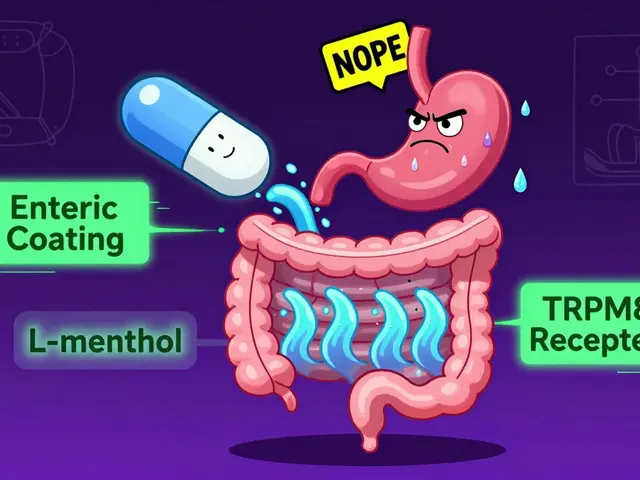
If you’ve tried two statins and still can’t handle them, you’re not out of options. There are proven, effective non-statin therapies. Here’s what works:- Ezetimibe (10mg daily): Reduces LDL by 18%. Takes effect in days. Side effects? Less than 5%-mostly mild bloating. It’s well tolerated in 94% of patients after 12 months. Often used with low-dose statins, but works alone too.
- Bempedoic acid (180mg daily): Lowers LDL by 17%. Designed for people who can’t take statins. Works in the liver, not the muscles. In trials, 88% stuck with it for a year. One study showed it reduced heart attacks by 23% in statin-intolerant patients.
- PCSK9 inhibitors (evolocumab, alirocumab): Injected every 2 or 4 weeks. Drops LDL by 59%. Used in high-risk patients with very high cholesterol. Adherence is 91%. Cost is high-around $5,800 a year-but insurance often covers it if you’ve tried other options.
- Bile acid sequestrants (colesevelam): Powder or tablet. Lowers LDL by 15-18%. Can cause constipation or gas in 22% of users. Good for those who can’t take pills with meals.
- Inclisiran: A twice-yearly injection that silences a liver gene to lower LDL. In trials, it cut LDL by 50% with 93% adherence. Approved in Europe and coming to the U.S. soon.
What About CoQ10, Diet, or Exercise?
You’ve probably heard that CoQ10 supplements help with statin muscle pain. The science? Weak. In double-blind trials, only 34% of people reported improvement. That’s no better than placebo. It’s not a reliable fix. Diet and exercise? They help-but not enough on their own. If your LDL is over 190 mg/dL, lifestyle changes alone won’t get you to goal. Statins (or alternatives) are still needed for people with heart disease, diabetes, or very high cholesterol. But combining them? That’s powerful. One study showed that patients who switched from statins to ezetimibe + bempedoic acid + a Mediterranean diet saw LDL drop 45% and reported fewer muscle symptoms than when they were on statins.
How to Get a Proper Diagnosis
If you think you’re statin intolerant, here’s what to ask your doctor:- Have I tried at least two different statins? One at the lowest dose?
- Did my symptoms go away after stopping the statin?
- Have we checked for other causes? (Vitamin D, thyroid, arthritis, fibromyalgia)
- Have we tried re-challenging? (Reintroducing the statin after a break to see if symptoms return?)
- Am I on a lipophilic statin? Could I switch to a hydrophilic one?
What’s Next for Statin Intolerance?
The field is changing fast. By 2025, genetic testing for the SLCO1B1 gene variant may be routine. People with the *5 or *15 allele have a 4.5 times higher risk of muscle side effects. Knowing this before starting a statin could prevent problems entirely. New drugs are coming too. Oral PCSK9 inhibitors (like MK-0616) are in Phase 3 trials. They work like the injectables but are pills. Inclisiran is already approved in Europe. And a new muscle-protecting drug called IMOD3001 is showing promise in early trials. The bottom line? Most people labeled as “statin intolerant” can be helped. Studies show over 90% of them can reach their cholesterol goals with the right combination of drugs and strategies. You don’t have to live with high cholesterol just because you had a bad experience with one pill.What to Do Today
Don’t stop your statin without talking to your doctor. If you’re having muscle symptoms:- Write down when they started, where they hurt, and how bad they are.
- Check your vitamin D level. If it’s under 30 ng/mL, supplementing may help.
- Ask if you can switch to rosuvastatin 5mg or pravastatin 10mg.
- Request ezetimibe if you’re still having issues.
- Don’t accept “just live with it” as an answer. There are better options.