QT Interval Calculator
Methadone Risk Assessment Tool
Calculate your QTc interval and assess risk level based on methadone treatment guidelines.
QTc Result
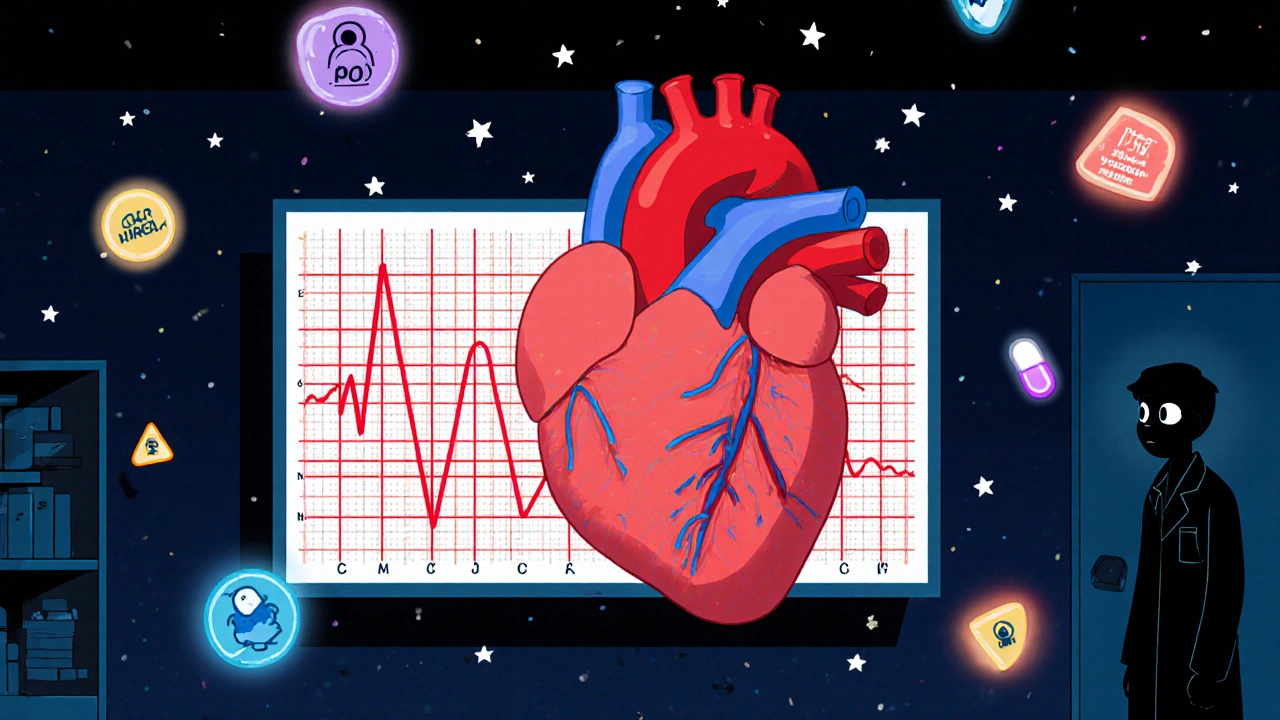
When you start methadone for opioid dependence, you’re not just getting relief from withdrawal. You’re also taking on a quiet, invisible risk-one that doesn’t show up in cravings or mood swings, but in the electrical rhythm of your heart. Methadone can stretch out the QT interval on your ECG, and if it goes too far, it can trigger a deadly heart rhythm called Torsades de Pointes. This isn’t theoretical. It’s real. And it’s preventable with the right monitoring.
Why Methadone Affects Your Heart
Methadone doesn’t just bind to opioid receptors. It also blocks a specific potassium channel in heart cells called hERG (KCNH2). This channel is responsible for resetting the heart’s electrical charge after each beat. When it’s blocked, the heart takes longer to recover. That delay shows up on an ECG as a longer QT interval. The longer the QT, the higher the chance of a dangerous arrhythmia. This isn’t a rare side effect. Studies show that between 9% and 88% of people on methadone have some degree of QT prolongation. The risk isn’t random-it’s tied to dose, other medications, and your body’s unique biology. And while sudden cardiac death from this is still uncommon, the consequences are fatal when they happen. Most cases occur in people taking high doses, but even lower doses can be risky if other factors line up.What’s a Normal QT Interval?
Not all QT prolongation is the same. Doctors use a corrected version called QTc, which adjusts for heart rate. Here’s what matters:- Normal: ≤430 ms for men, ≤450 ms for women
- Borderline: 431-450 ms (men), 451-470 ms (women)
- Significant prolongation: >450 ms (men), >470 ms (women)
- High risk: >500 ms - this quadruples your chance of sudden death
Who’s at Highest Risk?
Not everyone on methadone needs monthly ECGs. But some people are walking a tightrope. Here are the key risk factors that stack up:- Female gender - women have 2.5 times higher risk than men
- Age over 65 - older hearts don’t recover as easily
- Low potassium (<3.5 mmol/L) or low magnesium (<1.5 mg/dL)
- Heart disease - especially heart failure or past heart attack
- Slow heart rate (under 50 bpm)
- Already having long QT syndrome
- Taking other QT-prolonging drugs - like certain antidepressants, antipsychotics, or antibiotics
Drug Interactions That Make It Worse
Many people on methadone are also on meds for mental health, pain, or infections. Some of those drugs don’t just add up - they multiply the risk. Drugs that inhibit the CYP3A4 liver enzyme - like fluconazole (a fungus treatment), voriconazole, or the antidepressant fluvoxamine - can boost methadone levels in your blood by up to 50%. That’s not a minor interaction. That’s a cardiac emergency waiting to happen. Even common antibiotics like moxifloxacin or antipsychotics like haloperidol can push QT prolongation over the edge. If you’re on methadone, always tell every doctor - including your dentist - what you’re taking. A simple script for a sinus infection could set off a chain reaction.When and How to Monitor Your ECG
The good news? You don’t need endless ECGs. You need smart ones.- Baseline ECG: Before you start methadone - or before any dose increase
- Steady-state ECG: 2-4 weeks after starting or changing dose - this is when methadone levels stabilize
- Follow-up frequency: Based on your risk level
| Risk Level | QTc Range | Additional Risk Factors | Monitoring Frequency |
|---|---|---|---|
| Low Risk | <450 ms (men), <470 ms (women) | None | Every 6 months |
| Moderate Risk | 450-480 ms (men), 470-500 ms (women) | 1-2 factors (e.g., age, low potassium) | Every 3 months |
| High Risk | >480 ms (men), >500 ms (women) | 3+ factors or QTc >500 ms | Monthly - consider dose reduction or switch to buprenorphine |
Real-World Data Shows Monitoring Saves Lives
A 2017 study of 127 patients in a Swiss hospital found nearly 30% had QTc prolongation. Almost 9% were above 500 ms - a silent ticking bomb. The study pinpointed three key predictors: daily methadone dose over 100 mg, potassium under 4 mmol/L, and taking psychotropic drugs. But here’s the hopeful part: a 2023 study in JAMA Internal Medicine showed clinics that put in structured ECG protocols cut serious cardiac events by 67%. That’s not a small win. That’s life-saving. And it’s not just about the numbers. Patients who got regular ECGs said they felt safer - 82% reported confidence in their treatment, compared to just 47% of those who didn’t get monitored. Trust matters. Knowing your heart is being watched makes a difference.
What You Should Do Now
If you’re on methadone, here’s your action list:- Ask for a baseline ECG before starting or changing your dose
- Get a repeat ECG at 2-4 weeks after any dose change
- Know your QTc number - don’t let your provider just say “it’s fine”
- Get your potassium and magnesium checked at least every 3 months
- Make a list of every medication you take - including OTC and herbal - and review it with your prescriber
- If you’re over 65, female, or on high doses, insist on quarterly ECGs
- If your QTc is over 500 ms, ask about switching to buprenorphine
Why This Isn’t Just a ‘Drug Problem’
For years, sudden deaths in people on methadone were written off as overdose or complications of drug use. But the FDA’s 2006 warning made it clear: this is a cardiac issue. And it’s underdiagnosed. In the UK and US, methadone clinics vary wildly in how they monitor patients. Some have strict protocols. Others don’t do ECGs at all. That inconsistency puts lives at risk. You can’t rely on luck. You have to be your own advocate. Sleep apnea is another hidden factor - it affects about half of people on methadone. Nightly drops in oxygen can stress the heart and make QT prolongation worse. If you snore loudly or wake up gasping, get tested for sleep apnea. Treating it might lower your cardiac risk as much as adjusting your dose.What’s Next?
The science is clear. Monitoring saves lives. But it only works if it’s done consistently. If your clinic doesn’t have a written protocol for ECG monitoring, ask why. If they say it’s not necessary for low doses, push back - especially if you have any risk factors. Buprenorphine is a powerful alternative. It doesn’t carry the same QT risk. And for many people, it’s just as effective. If you’re high-risk and stuck on methadone, ask about switching. You’re not giving up - you’re choosing safety. Your recovery is about more than staying off opioids. It’s about living - not just surviving. And that means protecting your heart as much as your mind.Can methadone cause sudden death even at low doses?
Yes. While the risk is higher with doses over 100 mg/day, sudden cardiac death has occurred at lower doses - especially when combined with other risk factors like low potassium, female gender, or taking other QT-prolonging drugs. There’s no completely safe dose if multiple risks are present.
How often should I get an ECG if I’m on methadone?
It depends on your risk level. Low-risk patients (no risk factors, QTc under 450/470 ms) need an ECG every 6 months. Moderate-risk patients (one or two risk factors, QTc 450-500 ms) should be monitored every 3 months. High-risk patients (QTc over 500 ms or three or more risk factors) need monthly ECGs and should consider switching to buprenorphine.
What if my clinic won’t do regular ECGs?
If your clinic doesn’t follow standard guidelines, ask for a referral to a cardiologist or a different treatment center. You have the right to safe care. You can also request your own ECG through your GP - many primary care clinics will do it if you explain the cardiac risk. Don’t accept silence as an answer.
Can electrolyte imbalances cause QT prolongation on methadone?
Absolutely. Low potassium (under 3.5 mmol/L) and low magnesium (under 1.5 mg/dL) are major triggers. Methadone doesn’t directly lower these - but if you’re vomiting, sweating heavily, on diuretics, or eating poorly, your levels can drop fast. Get them checked every 3 months, and consider a potassium-rich diet (bananas, spinach, potatoes) if your levels are borderline.
Is buprenorphine really safer than methadone for the heart?
Yes. Multiple studies show buprenorphine has minimal to no effect on the QT interval, even at high doses. It’s just as effective for treating opioid dependence and has a lower overdose risk. If you have risk factors for QT prolongation, switching to buprenorphine is one of the safest choices you can make.
Does sleep apnea make methadone more dangerous for the heart?
Yes. About half of people on methadone have undiagnosed sleep apnea. Nightly drops in oxygen stress the heart and can worsen QT prolongation. If you snore, feel tired during the day, or wake up gasping, get tested. Treating sleep apnea with CPAP can reduce cardiac risk as much as lowering your methadone dose.
Are there any symptoms I should watch for?
Usually, there are none. QT prolongation doesn’t cause pain, dizziness, or palpitations until a dangerous arrhythmia starts - and by then, it’s often too late. That’s why regular ECGs are critical. Don’t wait for symptoms. If you feel faint, dizzy, or have a racing heartbeat, seek help immediately - but don’t rely on symptoms to tell you when you’re at risk.





Comments
John Kang
November 4, 2025 AT 00:34 AMBeen on methadone for 6 years now and never had an ECG until my nurse pushed me last year
Turns out my QTc was 485
They lowered my dose by 10mg and I’m fine now
Don’t wait for symptoms, get checked
Bob Stewart
November 5, 2025 AT 14:05 PMMethadone-induced QT prolongation is mediated by hERG potassium channel blockade which delays ventricular repolarization
QTc thresholds above 500 ms confer a fourfold increased risk of torsades de pointes
Guidelines from the American Heart Association recommend baseline and follow-up ECGs at 30 and 90 days for patients on doses exceeding 100 mg/day
Simran Mishra
November 6, 2025 AT 00:55 AMI remember the day I found out my QT was stretched too far
I sat in that clinic chair and just stared at the screen like it was a mirror showing my soul
I thought I was just getting my life back
Turns out I was dancing with death and no one told me
My mom cried when I told her
My doctor shrugged and said it’s common
Common doesn’t mean safe
Common doesn’t mean you won’t be the one
It doesn’t matter how many people it happens to
When it happens to you it’s the only thing that matters
I stopped taking it for two weeks
My body screamed
My mind screamed
But my heart… my heart was quiet for the first time in years
Now I take half the dose
And I get an ECG every month
And I still wake up some nights wondering if today’s the day
But at least I’m awake enough to check
Holly Lowe
November 6, 2025 AT 23:01 PMMethadone ain’t just a crutch-it’s a tightrope walk with a heartbeat as your only safety net
Some folks treat it like a magic pill but nah, it’s more like juggling chainsaws while blindfolded
That QT interval? That’s your heart’s SOS signal
Don’t ignore it just because you feel ‘fine’
Fine is a lie you tell yourself when you’re too scared to face the truth
Get that ECG. Do the work. Live longer. Period.
Sarah Khan
November 8, 2025 AT 00:31 AMThere’s something deeply ironic about using a drug to heal addiction while quietly risking death through its mechanism of action
We treat the mind but forget the body is still a biological system governed by physics and ion channels
It’s not malice that causes this-it’s systemic neglect
People on methadone are often invisible to the medical establishment until they collapse
And then it’s too late
Why do we wait for tragedy to validate prevention?
Why is monitoring optional when the stakes are death?
Maybe because addiction is still seen as a moral failure, not a medical condition
But your heart doesn’t care about your past-it only cares about potassium levels and QT intervals
And if we’re going to offer this treatment, we owe it to people to protect them from its hidden dangers
Not just in theory
But in practice
Every single time
Kelly Library Nook
November 8, 2025 AT 18:45 PMAnyone prescribing methadone without mandatory baseline and 30-day ECGs is practicing negligent medicine
There is no justification for delaying cardiac monitoring when the risk is well-documented, dose-dependent, and preventable
Failure to comply with standard of care constitutes malpractice
Stop treating this like a suggestion. It’s a requirement.
Charity Peters
November 9, 2025 AT 09:42 AMMy cousin died from this. No warning. Just gone.
Got his ECG back two days after. QTc was 520.
He never even knew.
Faye Woesthuis
November 11, 2025 AT 09:39 AMIf you’re on methadone and haven’t had an ECG, you’re not managing your health-you’re gambling with your life.
Stop being lazy.
Get tested.
raja gopal
November 11, 2025 AT 19:10 PMI’ve been clean for 11 years now on low-dose methadone
My heart’s been fine because I listen to my doctor
And I check my potassium every month
It’s not hard
It’s just care
You deserve that much
Samantha Stonebraker
November 13, 2025 AT 01:56 AMIt’s funny how we celebrate the courage it takes to walk into a clinic
But we ignore the quiet courage it takes to show up for your own heartbeat
Every ECG is a love letter to your future self
Don’t skip it
Even if you feel fine
Even if you’re tired
Even if the system makes it hard
Your heart doesn’t care about bureaucracy
It just wants to keep beating
Suryakant Godale
November 14, 2025 AT 19:02 PMAccording to the 2022 FDA safety communication, methadone-related QT prolongation is more prevalent in patients with concomitant use of CYP3A4 inhibitors, hypokalemia, or structural heart disease
Baseline ECG is recommended prior to initiation and within 30 days of dose escalation
Serial monitoring every 3–6 months is advised for patients with risk factors or QTc >450 ms
ka modesto
November 16, 2025 AT 14:33 PMBig shoutout to the nurses who actually check on this stuff
Most of us don’t even know what QT means
But my nurse sat me down with a diagram and said ‘this could kill you’
That changed everything
Thanks, Karen
You’re the real MVP
Cindy Burgess
November 17, 2025 AT 22:10 PMSo… we’re supposed to get an ECG every time they change the dose?
That’s a lot of appointments.
And what if I don’t have insurance?
Is this just another way to make poor people jump through hoops?
Or is it actually helpful?
Just asking.
Tressie Mitchell
November 18, 2025 AT 20:52 PMOf course you’re going to get QT prolongation-you’re on a synthetic opioid that’s essentially a chemical sledgehammer to your cardiac system.
And yet you’re surprised?
People who take methadone for ‘lifestyle reasons’ deserve exactly what they get.
It’s not the drug’s fault.
It’s yours.
dayana rincon
November 20, 2025 AT 11:18 AMQTc >500? 😬
That’s not a number, that’s a Netflix documentary waiting to happen
Get your ECG, babe. Your heart’s not a suggestion. 🫀🩺