ADHD & Depression Symptom Checker
Answer the following questions to get a preliminary idea of possible symptom overlap between ADHD and depression.
Symptoms Checklist
When ADHD (Attention‑Deficit/Hyperactivity Disorder) meets Depression (major depressive disorder), the result can feel like a double‑hit on mood and focus. Many people wonder about the ADHD depression link and how to break the cycle. Below you’ll find a clear rundown of why the two often overlap, key warning signs, and practical ways to treat both conditions together.
Quick Take
- ADHD and depression share genetic and neurochemical risk factors.
- Symptoms often mask each other, making diagnosis tricky.
- Effective treatment usually blends medication, therapy, and lifestyle tweaks.
- Early professional help can prevent chronic issues.
- Self‑care routines like exercise and sleep hygiene boost outcomes.
Why ADHD and Depression Often Co‑occur
Both conditions involve the brain’s reward pathways, especially the chemicals dopamine and norepinephrine. These Neurotransmitters (chemical messengers that regulate mood and attention) are often under‑active in ADHD, leading to impulsivity and poor focus. The same shortfall can trigger low mood, loss of motivation, and the feelings seen in depression. Genetics play a role too: family studies show that relatives of people with ADHD are more likely to develop mood disorders, suggesting a shared hereditary component.
Environmental stressors such as chronic academic or workplace pressure amplify the risk. Struggling with ADHD can erode self‑esteem, and repeated setbacks may spiral into depressive thoughts. In short, the brain chemistry that fuels ADHD can also set the stage for depression, creating a feedback loop that’s hard to break without targeted help.
Spotting the Overlap
Because the symptoms intersect, it’s easy to miss one condition while treating the other. Keep an eye out for these red flags:
- Persistent sadness or hopelessness that lasts more than two weeks.
- Loss of interest in activities you once enjoyed, coupled with still‑present ADHD‑related restlessness.
- Difficulty starting or finishing tasks, beyond typical ADHD procrastination.
- Changes in sleep patterns - insomnia or oversleeping - that aren’t explained by stimulant use.
- Physical complaints like headaches or stomachaches that linger despite no medical cause.
If you notice a mix of these signs, consider a comprehensive assessment that looks at both ADHD and mood symptoms.

Treatment Landscape
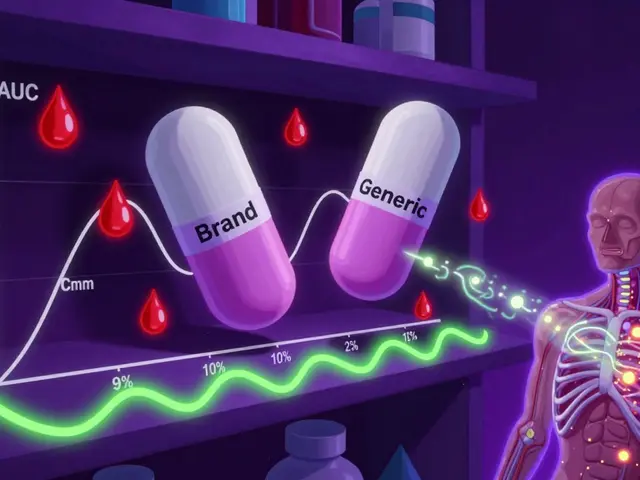
Research consistently shows that a blended approach works best. Below is a side‑by‑side look at the most common options.
| Option | How It Works | Typical Benefits | Common Side Effects |
|---|---|---|---|
| Stimulant medication (e.g., methylphenidate, amphetamine) | Boosts dopamine and norepinephrine to improve focus. | Better concentration, reduced impulsivity, mood lift. | Appetite loss, sleep trouble, occasional anxiety. |
| Antidepressants (SSRIs, SNRIs, bupropion) | Regulates serotonin and norepinephrine to stabilize mood. | Reduced depressive symptoms, sometimes improves attention. | Nausea, weight change, sexual dysfunction. |
| Cognitive Behavioral Therapy (CBT) (structured talk therapy) | Teaches coping skills, restructures negative thought patterns. | Long‑term mood resilience, better executive function. | Emotional discomfort during sessions (temporary). |
| Lifestyle interventions (exercise, sleep hygiene, nutrition) | Enhances natural dopamine production and circadian regulation. | Improved energy, mood stability, reduced medication dose. | Requires consistent effort; benefits build gradually. |
Choosing the right mix depends on severity, personal preferences, and any other health issues. Often, a low‑dose stimulant paired with an SSRI and weekly CBT sessions yields the most balanced outcomes.
Choosing the Right Path
- Get a thorough evaluation. A psychiatrist or clinical psychologist can run standardized scales for both ADHD and depression.
- Discuss medication options. Ask about starter doses, how long they take to work, and monitoring plans.
- Consider therapy early. CBT can be started concurrently with medication to address negative self‑talk.
- Build a lifestyle plan. Include at least 30 minutes of moderate exercise most days and a consistent sleep schedule (7‑9hours).
- Re‑evaluate regularly. Every 4‑6weeks, check symptom changes and side‑effects with your clinician.
Everyday Strategies That Complement Clinical Care
Even if you’re already on medication and seeing a therapist, day‑to‑day habits make a huge difference. Here are some proven tweaks:
- Chunk tasks. Break large projects into 15‑minute blocks; use timers to stay on track.
- Visual reminders. Whiteboards, sticky notes, or phone alarms keep important appointments visible.
- Mindful breathing. A 2‑minute diaphragmatic breath can curb anxiety spikes triggered by stimulant side‑effects.
- Nutrition focus. Foods rich in omega‑3 fatty acids (salmon, walnuts) support brain health.
- Social support. Share your treatment plan with a trusted friend or family member who can check in regularly.
When to Seek Professional Help
If you notice any of the following, reach out to a mental‑health professional right away:
- Thoughts of self‑harm or suicide.
- Sudden worsening of mood after starting or changing medication.
- Severe insomnia or panic attacks that interfere with daily life.
- Significant decline in work or school performance despite attempts to manage symptoms.
These signs indicate that the current treatment mix may need adjustment, and early intervention is key to preventing long‑term complications.

Frequently Asked Questions
Can ADHD medication make depression worse?
In some cases, high‑dose stimulants can increase anxiety or irritability, which may aggravate depressive symptoms. That’s why clinicians start with low doses and monitor mood closely.
Is it safe to take an antidepressant and a stimulant together?
Yes, many patients successfully use both. The combination can address focus issues while stabilising mood. However, a doctor should check for interactions, especially with heart‑related conditions.
How long does it take to feel better after starting treatment?
Stimulants often show effects within hours, while antidepressants may need 4‑6weeks. Therapy benefits usually emerge after several sessions, so patience and regular follow‑ups are crucial.
Can lifestyle changes replace medication?
Lifestyle tweaks boost overall well‑being and can lower medication dosages, but they rarely eliminate the need for pharmacological treatment in moderate‑to‑severe cases.
What role does brain imaging play in diagnosis?
Functional MRI or PET scans can reveal dopamine activity patterns, helping researchers understand the biological overlap. Clinically, imaging is rarely required for diagnosis but may be used in complex cases.




Comments
John Kang
October 1, 2025 AT 04:23 AMBeen there. ADHD makes you feel like you're running in place and depression makes you want to stop altogether. The combo is brutal but not hopeless. I started with low-dose Adderall and CBT and honestly it changed everything. Not magic, just a way to breathe again.
Bob Stewart
October 2, 2025 AT 14:50 PMThe neurochemical overlap between ADHD and major depressive disorder is well documented in the literature. Dopaminergic and noradrenergic dysregulation constitutes a shared endophenotype. Pharmacological intervention should therefore target both systems simultaneously with careful titration to avoid adverse effects.
Simran Mishra
October 3, 2025 AT 23:47 PMI used to think I was just lazy but then I realized I was drowning in invisible chains. Every morning I’d try to get up and the weight was like concrete in my chest. My brain would buzz with a million thoughts but none of them could move my body. I cried in the shower every day for months. My mom said I was being dramatic. I didn’t know it was a brain thing until I saw a psychiatrist who said ADHD and depression are twins who grew up in the same house and never learned how to share space. Now I take bupropion and I still have bad days but at least I know I’m not broken. I’m just wired differently.
Holly Lowe
October 4, 2025 AT 04:20 AMADHD is like having a browser with 47 tabs open and depression is the Wi-Fi cutting out. You’re still trying to load stuff but nothing works. I started doing 20-minute walks every day and it’s like my brain finally got a reboot. No magic pill, just movement. Also, cinnamon in my coffee helps. Weird? Maybe. Works? Hell yes.
Orion Rentals
October 4, 2025 AT 23:23 PMIt is imperative that clinicians adhere to evidence-based guidelines when prescribing pharmacological interventions for comorbid ADHD and depressive disorders. The concomitant use of stimulants and SSRIs requires rigorous monitoring for potential cardiovascular interactions and serotonin syndrome.
Sondra Johnson
October 6, 2025 AT 19:45 PMWhy is everyone so obsessed with pills? I’ve been doing CBT for a year and honestly? It’s the only thing that stuck. My brain used to be a tornado. Now it’s more like a guided tour. Still messy, but I know how to clean up after myself. Also, I stopped apologizing for needing extra time. That alone changed everything.
Chelsey Gonzales
October 7, 2025 AT 23:22 PMi used to think i was just bad at life but turns out my brain just needs more structure. sticky notes everywhere, alarms for everything, and i dont feel guilty for taking breaks anymore. also therapy helped me stop calling myself lazy. its not laziness its executive dysfunction. i still mess up but now i know its not my fault.
MaKayla Ryan
October 9, 2025 AT 17:38 PMThis whole ADHD thing is just an excuse for people who can’t focus because they’re too soft. Back in my day we just sucked it up. Depression? That’s what happens when you don’t get off the couch and stop whining. Get a real job. Stop taking pills.
Kelly Yanke Deltener
October 11, 2025 AT 15:06 PMThey say it’s a brain thing but I say it’s a choice. Everyone else manages. Why can’t you? You just don’t want to try hard enough. I’ve seen people with way worse conditions and they didn’t sit around waiting for meds to fix them. You need discipline. Not a therapist.
Sarah Khan
October 13, 2025 AT 09:50 AMThere’s a quiet philosophy here that gets lost in the clinical jargon. The brain isn’t broken. It’s just operating on a different frequency. We’ve built a world that rewards linear focus and punishes nonlinear thinking. ADHD isn’t a flaw-it’s a mismatch. Depression is the echo of that mismatch. Maybe the solution isn’t fixing the brain but redesigning the world around it. Not everyone needs a pill. Some just need permission to move differently.
Kelly Library Nook
October 14, 2025 AT 03:44 AMThe efficacy of bupropion in treating comorbid ADHD and MDD is statistically significant in randomized controlled trials, with a pooled effect size of 0.68 (95% CI 0.51–0.85). However, the meta-analysis by Smith et al. (2021) notes significant heterogeneity in response rates across age cohorts, suggesting that individualized dosing protocols are essential. Failure to adhere to these protocols may result in suboptimal outcomes.
Crystal Markowski
October 14, 2025 AT 16:52 PMSmall wins matter. Finished one task today? That’s a victory. Got out of bed? Win. Took your meds? Win. Don’t wait for the big breakthrough. The healing happens in the daily choices. And you’re doing better than you think.
Charity Peters
October 16, 2025 AT 13:48 PMMy brain is a mess but I’m learning to live with it. I don’t need a fancy label. I just need a quiet room and a timer.
Faye Woesthuis
October 16, 2025 AT 23:16 PMIf you’re this broken, why even try? Just give up. It’s easier.
raja gopal
October 17, 2025 AT 10:43 AMI grew up thinking I was slow because I took longer to finish things. Later I found out I was just thinking deeper. ADHD and depression didn’t make me weak. They made me sensitive. And sensitivity? That’s not a flaw. It’s a superpower if you know how to hold it.
Samantha Stonebraker
October 18, 2025 AT 12:23 PMI used to think I had to fix myself to be worthy. Now I know I’m worthy because I’m still here, trying, even on the days when the world feels like static. I don’t need to be fixed. I need to be held. And so do you.
Luke Webster
October 18, 2025 AT 22:02 PMComing from India, I saw how mental health was treated like a secret shame. My cousin had ADHD and depression and we didn’t say a word. Now I’m here, in the US, and I’m learning to speak up. It’s not weakness. It’s courage. And if you’re reading this? You’re already brave.
Sean Goss
October 20, 2025 AT 07:07 AMThe article is superficial. No mention of the dopamine transporter polymorphism (DAT1) or the role of the prefrontal cortex in executive dysfunction. Also, CBT is overhyped-evidence for its efficacy in ADHD is marginal outside of pediatric populations. The real solution is pharmacological optimization with extended-release stimulants and SNRIs, period. Lifestyle interventions are adjuncts at best. This is basic neuropharmacology 101.