When your hands swell up in the morning, your knees ache for no clear reason, and your joints feel stiff even after resting, it’s not just aging or overuse. For nearly 9 out of 10 people with systemic lupus erythematosus (SLE), this is lupus arthritis-a persistent, inflammatory type of joint pain that doesn’t destroy bone like rheumatoid arthritis, but still steals mobility and quality of life.
What Makes Lupus Arthritis Different?
Lupus arthritis isn’t the same as osteoarthritis or even typical rheumatoid arthritis. It hits the small joints-fingers, wrists, knuckles, and sometimes knees-symmetrically, meaning if one hand is affected, the other usually is too. But unlike rheumatoid arthritis, it rarely causes permanent joint damage or bone erosion. The inflammation comes from the immune system attacking the body’s own tissues, triggered by abnormal activation of immune cells called dendritic cells and macrophages. This leads to excess cytokines like TNF-alpha and interleukin-6 flooding the joints, causing swelling, warmth, and pain that comes and goes in waves.What makes it tricky is that lupus arthritis often hides behind other symptoms: fatigue, rashes, fever, or kidney issues. Many patients assume their joint pain is just part of being tired or stressed. But when it’s persistent, symmetrical, and doesn’t improve with rest, it’s a red flag for lupus. Studies show that up to 90% of SLE patients will develop joint inflammation at some point, often early in the disease.
Why Hydroxychloroquine Is the First-Line Treatment
Hydroxychloroquine, sold under the brand name Plaquenil, isn’t a painkiller. It doesn’t numb the ache like ibuprofen or naproxen. Instead, it works at the root-calming the overactive immune system that’s causing the inflammation in the first place. Since the 1950s, doctors have known it helps lupus patients, but only in the last 20 years have we understood exactly how.Hydroxychloroquine blocks key immune sensors called Toll-like receptors (TLR7 and TLR9), which normally detect viruses and bacteria. In lupus, these receptors get tricked into thinking the body’s own DNA is an invader. When they’re overactive, they trigger a cascade of inflammation. Hydroxychloroquine lowers this signal by 35-40%, reducing interferon levels and calming the immune storm. It also cuts down on TNF-alpha and interleukin-6 by 20-30%, directly reducing joint swelling and pain.
But its benefits go beyond joints. Hydroxychloroquine lowers the risk of blood clots by 30-35% in patients with antiphospholipid syndrome-a common lupus complication. It improves cholesterol levels, raising good HDL and lowering bad LDL. It even helps protect the heart: one Johns Hopkins study of over 2,000 lupus patients found those on hydroxychloroquine had a 44% lower risk of heart attacks and strokes over 20 years.
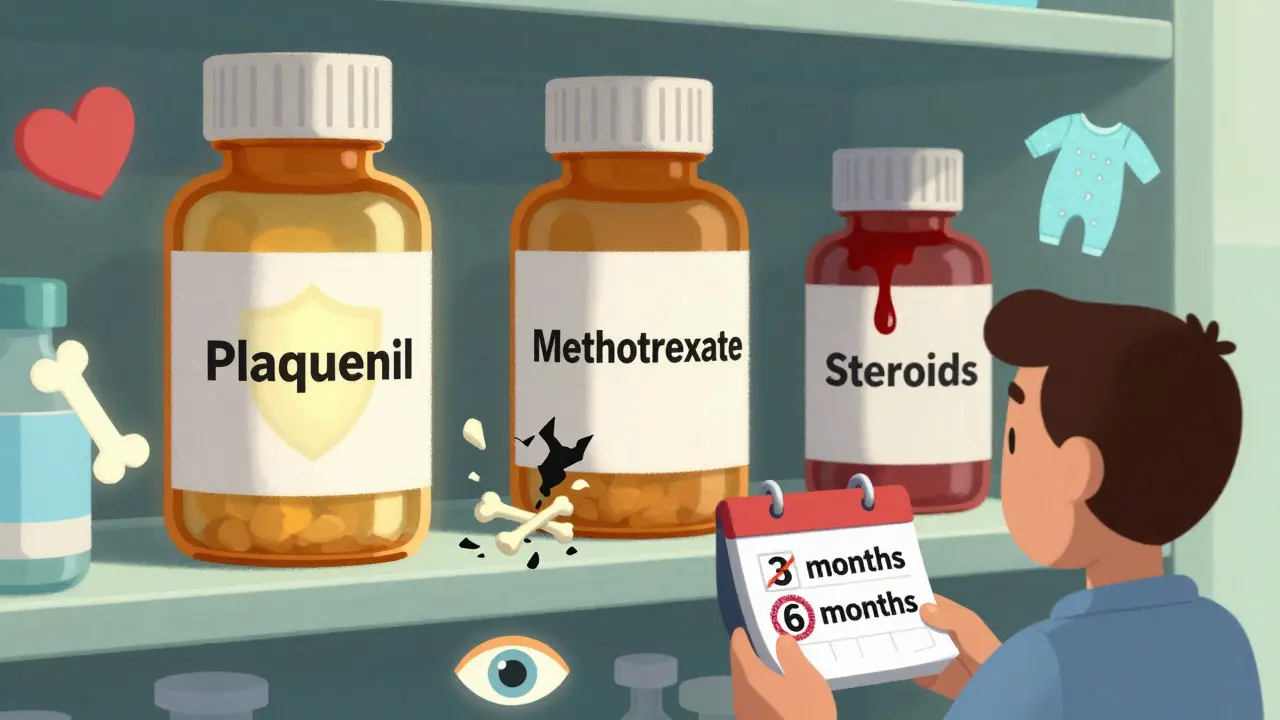
How Long Does It Take to Work?
This is where many patients get discouraged. Hydroxychloroquine doesn’t work overnight. Unlike steroids, which can reduce swelling in days, hydroxychloroquine takes 3 to 6 months to show real results. Some people notice small improvements at 8 weeks, but the full effect usually takes half a year.A 2018 study tracking 1,200 lupus patients found that only 62% saw measurable improvement in joint counts by 12 weeks. By 6 months, that number jumped to 85%. That delay is why so many patients stop taking it too soon-up to 25% quit within the first year because they don’t feel immediate relief. But those who stick with it often report life-changing results: reduced steroid use, fewer flares, and better overall function.
One patient on the Lupus Foundation forum wrote: “After four months on 300mg of Plaquenil, I went from needing 10mg of prednisone daily to zero. My morning stiffness vanished.” That’s not rare. In a survey of 3,542 lupus patients, 76% said hydroxychloroquine reduced joint swelling, and 68% reported fewer flares.
Dosing and Safety: What You Need to Know
The dose isn’t one-size-fits-all. It’s based on your real body weight: no more than 5 mg per kilogram per day. For most adults, that means 200-400 mg daily. A 62 kg person would typically take 300 mg. Taking more doesn’t make it work faster-it just increases risk.The biggest concern is eye damage. Hydroxychloroquine can rarely cause retinal toxicity, especially after 5+ years of use or if the dose is too high. That’s why annual eye exams are non-negotiable. The American Academy of Ophthalmology recommends a baseline eye test within the first year, then yearly after five years. New tools like the AdaptDx Pro dark adaptometer can detect early changes before vision loss occurs, cutting false negatives by 35%.
Other side effects are mild: nausea (30%), vivid dreams (45%), and occasional dizziness. These often fade after a few weeks. If nausea is bad, take the pill with food or split the dose. Don’t skip doses because you’re afraid of side effects-most are manageable.
One surprising benefit? Hydroxychloroquine may actually improve bone health. While long-term steroids cause osteoporosis, studies show hydroxychloroquine users gain 3-5% more bone density in the spine over two years. That’s huge for lupus patients, who are already at higher risk for bone loss.
How It Compares to Other Treatments
Many patients wonder: why not use methotrexate or biologics like belimumab instead?Methotrexate works faster for severe joint inflammation and can reduce swelling by 15-20% more than hydroxychloroquine. But it comes with risks: liver damage, low blood counts, and the need for monthly blood tests. Hydroxychloroquine? Just an annual eye exam and occasional blood work.
Biologics like belimumab reduce disease activity by 30-35%, but cost $45,000 a year. Hydroxychloroquine? Between $600 and $1,200 annually-even the brand-name Plaquenil costs less than $6 per pill. Generics are even cheaper, though some studies show certain generics have lower blood levels, so sticking with the same manufacturer matters.
Corticosteroids? They work fast-within 1-2 weeks-but long-term use increases infection risk, weight gain, diabetes, and bone loss. Hydroxychloroquine reduces the need for steroids by up to 50% in many patients.
That’s why guidelines from the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR) recommend hydroxychloroquine for every SLE patient, regardless of disease severity. It’s not just for joints-it’s for the whole body.
Real-World Challenges and How to Overcome Them
The biggest barrier isn’t the drug-it’s the patient experience. Waiting six months for results is hard. Fear of eye damage is real. And some doctors still don’t emphasize adherence enough.Patients who succeed on hydroxychloroquine share a few habits: they set phone reminders for pills, keep a symptom journal to track progress, and schedule eye exams without delay. The Lupus Foundation’s “Plaquenil Passport” program helps patients track doses and appointments. Over 15,000 people downloaded it in 2022.
Another issue: generic substitution. A 2022 JAMA study found some generic versions led to 18% lower blood levels than brand-name Plaquenil. If you notice your symptoms worsening after switching generics, talk to your doctor about switching back.
For pregnant patients, hydroxychloroquine is one of the safest options. The PROMISSE study showed no increased risk to babies, and 78% of pregnant lupus patients now take it to prevent flares and complications.
The Future of Hydroxychloroquine in Lupus
Research is still evolving. A 2023 study identified new biomarkers-like interferon gene signatures and TLR9 levels-that may predict who responds best to hydroxychloroquine. That could lead to personalized dosing in the future.Trials are now testing hydroxychloroquine combined with newer drugs like anifrolumab. Early results show a 45% better response rate than hydroxychloroquine alone. Even more exciting: scientists are finding it may influence gene expression and gut bacteria-suggesting its benefits go deeper than we thought.
For now, hydroxychloroquine remains the most studied, safest, and most widely used drug for lupus arthritis. It’s not a cure, but it’s the closest thing we have to a shield against the disease’s worst effects.
If you have lupus and haven’t tried hydroxychloroquine, ask your rheumatologist why. If you’re on it and not seeing results yet-don’t quit. Give it time. And never skip your eye checkups.
How long does hydroxychloroquine take to work for lupus arthritis?
Hydroxychloroquine typically takes 3 to 6 months to show noticeable improvement in joint pain and swelling. Some patients notice minor changes after 8-12 weeks, but the full benefit usually appears after six months. This delay is why adherence is critical-many patients stop too early, thinking it’s not working.
Is hydroxychloroquine safe for long-term use?
Yes, for most people. Hydroxychloroquine has a strong safety profile compared to steroids or immunosuppressants. The main long-term risk is retinal toxicity, which occurs in about 1 in 20 patients after 5+ years of use-especially if the dose exceeds 5 mg/kg/day. Annual eye exams and sticking to the correct weight-based dose reduce this risk dramatically. Other side effects like nausea or vivid dreams are usually mild and temporary.
Can I stop taking hydroxychloroquine if my symptoms improve?
No, not without consulting your doctor. Stopping hydroxychloroquine increases the risk of lupus flares by up to 50%. Even if your joints feel fine, the drug is still working to prevent inflammation in other organs like your kidneys, heart, and skin. Most patients stay on it indefinitely as a maintenance therapy.
Does hydroxychloroquine help with lupus fatigue?
Yes, many patients report improved energy levels after starting hydroxychloroquine. While it doesn’t directly stimulate energy, by reducing overall inflammation and lowering the frequency of flares, it helps the body recover more fully between episodes. Fatigue in lupus is often tied to chronic immune activation-hydroxychloroquine directly targets that.
Why is hydroxychloroquine preferred over methotrexate for lupus arthritis?
Methotrexate is stronger for active synovitis, but hydroxychloroquine is safer and offers broader protection. Methotrexate requires monthly blood tests, carries a higher risk of liver damage, and isn’t recommended during pregnancy. Hydroxychloroquine has fewer side effects, protects the heart and bones, reduces blood clots, and is safe for long-term use-even in children and pregnant women. It’s the foundation drug for lupus, not just for joints but for overall disease control.
Are generic versions of hydroxychloroquine as effective as Plaquenil?
Most generics are effective, but a 2022 study found some had 18% lower blood concentrations than brand-name Plaquenil. This can lead to reduced effectiveness or more flares. If you switch generics and notice your symptoms returning, talk to your doctor about switching back to the brand or a specific generic manufacturer known for consistent absorption.
Can hydroxychloroquine prevent lupus from developing in people at risk?
Some studies suggest it might. In people with positive autoantibodies but no diagnosed lupus, hydroxychloroquine lowered the risk of progressing to full SLE by 58% in one trial. But the 2022 ASAS PREVENT trial found no significant difference over 24 months. The evidence is mixed, so it’s not yet standard practice to prescribe it preventively-but research is ongoing.
What should I do if I experience vision changes while on hydroxychloroquine?
Stop taking the medication immediately and contact your rheumatologist and ophthalmologist. Early signs include blurred vision, difficulty focusing, or seeing light halos. Retinal damage from hydroxychloroquine is often irreversible, but catching it early can prevent further harm. Never ignore vision changes-even if they seem minor.







Comments
Phil Hillson
January 19, 2026 AT 01:56 AMLook I get it hydroxychloroquine is the new holy grail but let’s be real here this whole thing feels like Big Pharma’s way of keeping us on lifelong meds while they rake in billions
Malikah Rajap
January 20, 2026 AT 06:56 AMWait… so you’re telling me this drug that was once called a ‘covid hoax pill’ is now the gold standard for lupus? I’m not mad… just impressed… and slightly terrified.
Josh Kenna
January 20, 2026 AT 21:22 PMMy sister’s been on this for 3 years and her joints feel like they used to in high school-before the pain-before the meds-before everything changed. I wish I’d known this sooner. I almost lost her to a flare last winter.
Valerie DeLoach
January 21, 2026 AT 23:42 PMAs someone who’s lived with lupus for 17 years, I can say this: hydroxychloroquine didn’t just manage my arthritis-it gave me back my identity. I used to cancel plans because I couldn’t hold a coffee cup. Now I teach yoga to other patients. This drug doesn’t just treat-it transforms.
Christi Steinbeck
January 22, 2026 AT 12:35 PMDon’t let the 6-month wait scare you. I started at 200mg, added 100mg after 10 weeks, and by month 5 I was hiking again. It’s not magic-it’s medicine. And you deserve to feel like yourself again.
Lewis Yeaple
January 23, 2026 AT 15:55 PMWhile the pharmacological mechanisms are indeed compelling, one must acknowledge the substantial methodological limitations in the cited Hopkins cohort study, particularly regarding confounding by indication and immortal time bias. The 44% reduction in cardiovascular events is statistically significant but not necessarily causal.
Jacob Hill
January 24, 2026 AT 14:22 PMCan we talk about how the generics issue is a nightmare? I switched to a cheaper brand last year and my fatigue came back like a freight train. My rheumatologist said, ‘Just stick with Plaquenil.’ Worth every penny.
sujit paul
January 25, 2026 AT 23:21 PMIt is fascinating how the immune system, that intricate tapestry of cellular diplomacy, is manipulated by a molecule derived from the bark of the cinchona tree-yet modern medicine reduces this to a pill, a dosage, a timeline. We have forgotten that healing is not merely chemical-it is spiritual, temporal, and deeply personal.
Tracy Howard
January 27, 2026 AT 21:41 PMOf course Americans love this drug-because it’s cheap and doesn’t require surgery. In Canada, we have real treatments. Hydroxychloroquine? That’s what you give people when you don’t have the budget to treat them properly.
Aman Kumar
January 28, 2026 AT 03:19 AMLet me be blunt: if you're taking hydroxychloroquine without monitoring your interferon signature, TLR9 expression, and gut microbiome diversity, you're not managing lupus-you're gambling with your organs. Most doctors are still stuck in the 2010s.
Jake Rudin
January 29, 2026 AT 12:50 PMEvery time I hear someone say ‘just give it six months,’ I think of all the people who didn’t make it that far. Chronic illness isn’t a waiting game-it’s a war. And this drug? It’s the only shield we’ve got.
Jackson Doughart
January 31, 2026 AT 05:09 AMI’ve been on this for 8 years. No flares. No steroids. No hospital stays. My eyes are fine because I get checked every year. I’m not a hero. I just followed the rules. You can do this too.