After having a baby, many women feel exhausted, overwhelmed, and emotionally drained. It’s normal. But what if your fatigue isn’t just from sleepless nights? What if your hair is falling out, you’re gaining weight despite eating less, and you feel freezing cold when everyone else is warm? These aren’t just signs of being a new mom-they could be symptoms of postpartum thyroiditis, a hidden thyroid condition that affects 5 to 10% of women after childbirth.
What Exactly Is Postpartum Thyroiditis?
Postpartum thyroiditis is an autoimmune inflammation of the thyroid gland that happens within the first year after giving birth, miscarriage, or abortion. It’s not caused by an infection or a tumor. Instead, your immune system-still adjusting after pregnancy-mistakenly attacks your thyroid. This triggers a two-phase breakdown in thyroid function: first, too much hormone leaks out (hyperthyroidism), then your thyroid runs out of stored hormones and can’t make enough (hypothyroidism).
The condition is often mistaken for postpartum depression or just "normal" exhaustion. But the difference is physical. With thyroiditis, you’ll likely have measurable changes in your body: your heart races, you lose weight without trying, then later gain it back-and you feel like you’re running on empty even after eight hours of sleep.
The Two Phases: Hyperthyroidism Then Hypothyroidism
Most women go through two clear phases, though not everyone experiences both.
Phase 1: Hyperthyroidism (1-4 months postpartum)
This phase is often mild or even unnoticed. About half of women don’t even realize they’re in it. But if symptoms show up, they include:
- Heart rate over 100 beats per minute
- Feeling hot when others are cold
- Unintentional weight loss (4-7 pounds)
- Tremors in the hands
- Insomnia despite being exhausted
During this phase, your thyroid is leaking stored hormones because immune cells are damaging the gland. It’s not overactive like in Graves’ disease-it’s leaking. That’s why radioactive iodine uptake tests show levels below 2% (normal is over 60% in Graves’). This is a key clue doctors use to tell them apart.
Phase 2: Hypothyroidism (4-8 months postpartum)
This is when most women finally seek help. Symptoms are harder to ignore:
- Extreme fatigue (reported by 89% of affected women)
- Feeling cold all the time
- Constipation
- Dry, flaky skin
- Thinning hair or noticeable hair loss
- Brain fog-trouble focusing, remembering names, or making simple decisions
- Weight gain of 5-10 pounds without change in diet
Some women skip the hyperthyroid phase entirely and go straight into hypothyroidism. About 10-25% of cases are like this. Others only have the hyperthyroid phase and recover without ever becoming hypothyroid. But for most, the hypothyroid phase lasts 9-12 months.
How Is It Diagnosed?
There’s no single symptom that confirms it. Diagnosis relies on blood tests.
Your doctor should check:
- TSH (thyroid-stimulating hormone): High in hypothyroidism (>4.5 mIU/L), low in hyperthyroidism (<0.4 mIU/L)
- Free T4: Low in hypothyroidism, high in hyperthyroidism
- TPO antibodies: Present in 80-90% of cases. If these are high, you’re at much greater risk for permanent thyroid damage later.
Testing is most useful between 6 and 12 weeks after delivery, especially if you have risk factors like type 1 diabetes, a history of thyroid issues, or a family history of autoimmune disease. But many doctors don’t test unless you bring it up.
One woman in Bristol told her midwife she couldn’t get out of bed. She was told she was just "sleep-deprived." Three months later, after a panic attack and heart palpitations, she finally got tested. Her TSH was 18.5. Her TPO antibodies were off the charts. She had postpartum thyroiditis.
Who’s at Risk?
You’re more likely to get postpartum thyroiditis if you have:
- Type 1 diabetes (25-30% risk)
- Previous postpartum thyroiditis (40% chance of recurrence)
- High TPO antibody levels before or during pregnancy (70% risk)
- A personal or family history of Hashimoto’s or Graves’ disease
- Other autoimmune conditions like lupus or rheumatoid arthritis
Even if you don’t have any of these, you’re still at risk. About 5-10% of all women get it. That’s 1 in every 10-20 new moms. It doesn’t discriminate.
How Is It Treated?
Most cases resolve on their own. That’s the good news.
During the hyperthyroid phase: Usually, no treatment is needed unless symptoms are severe. If your heart is racing or you’re anxious, your doctor might prescribe a beta-blocker like propranolol to slow your heart rate and ease tremors. But you won’t get antithyroid drugs like methimazole-those are for Graves’ disease, not this.
During the hypothyroid phase: If your TSH is high and you have symptoms, you’ll likely be started on levothyroxine, a synthetic thyroid hormone. It’s safe, even while breastfeeding. Most women take it for 6-12 months. Then, after a repeat blood test, your doctor may slowly reduce the dose to see if your thyroid has recovered.
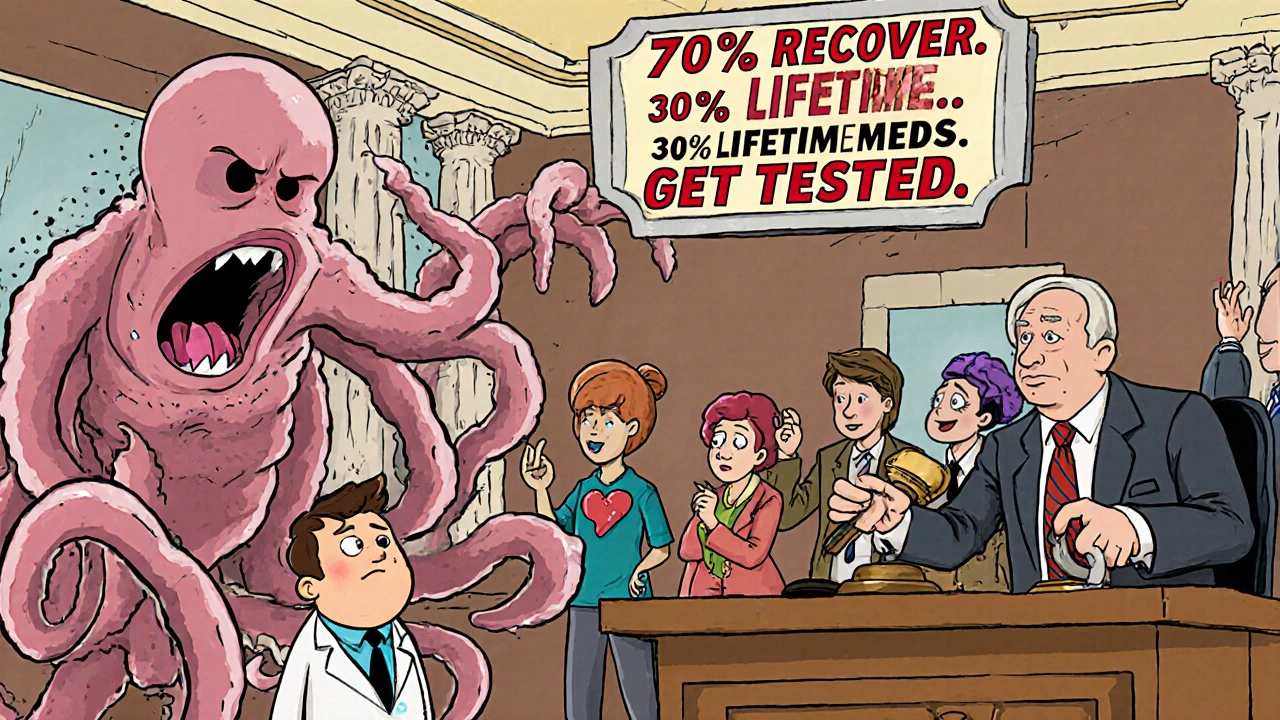
But here’s the catch: 20-30% of women never fully recover. Their thyroid stays underactive. They need lifelong levothyroxine. That’s why follow-up testing at 12 and 18 months is critical.
Why It Gets Missed-And Why That’s Dangerous
Doctors miss it because the symptoms look like postpartum depression. Fatigue, mood swings, brain fog-these are all shared. In fact, 30% of women with thyroiditis are initially misdiagnosed with depression and prescribed antidepressants. One study found 40% of these women were put on antidepressants before their thyroid was ever tested.
And it’s not just doctors. Many new moms think their symptoms are normal. They feel guilty for not enjoying motherhood. They push through the exhaustion. They don’t realize their body is fighting an invisible autoimmune battle.
Delayed diagnosis means longer suffering. On average, women wait 5.2 months before getting tested. In some cases, it takes three different doctors. Reddit threads are full of stories like: "I was told I was just tired. I cried for months. Then I found a doctor who listened. My TSH was 27. I had no idea."
What About Breastfeeding?
Levothyroxine is safe during breastfeeding. Only tiny amounts pass into breast milk, and studies show no effect on infant thyroid function. In fact, untreated hypothyroidism can reduce milk supply. So treating it often helps breastfeeding succeed.
If you’re struggling with low supply, check your thyroid. It’s one of the most common reversible causes.
What Happens Long-Term?
Good news: 70-80% of women return to normal thyroid function within 12-18 months. But 20-30% develop permanent hypothyroidism. That means lifelong medication.
Women with high TPO antibodies are far more likely to end up in this group. That’s why testing for antibodies isn’t just for diagnosis-it’s for future planning. If yours are high, you’ll need annual TSH checks even after recovery.
And here’s something most women don’t know: if you’ve had postpartum thyroiditis, your risk of developing Hashimoto’s or other autoimmune thyroid disease later in life jumps significantly. It’s not a one-time event. It’s a warning sign.
What Should You Do?
If you’re a new mom and your symptoms don’t improve after 3-4 months:
- Ask your doctor for a TSH and free T4 blood test.
- Ask for TPO antibody testing, especially if you have risk factors.
- Don’t accept "it’s just stress" or "you’re just tired."
- Keep a symptom journal: track sleep, energy, weight, mood, temperature sensitivity.
- If your doctor refuses, go to an endocrinologist or request a referral.
There’s no universal screening in the U.S. or U.K. yet. But awareness is growing. In Europe, 85% of countries screen high-risk women. In the U.S., only 42% of OB-GYNs routinely test beyond 12 weeks. That’s changing. Experts predict universal screening at 6 and 12 weeks will become standard within five years.
Final Thoughts
Postpartum thyroiditis isn’t rare. It’s overlooked. And that’s dangerous. Your body just went through one of the most physically demanding events of your life. Now it’s trying to reset. Sometimes, the reset fails. That doesn’t mean you’re broken. It means your immune system needs help.
If you’ve been told you’re just tired, but you feel like you’re running on fumes-get tested. It’s a simple blood draw. It takes five minutes. It could change everything.
You didn’t fail. Your thyroid did. And it can be fixed.
Is postpartum thyroiditis the same as postpartum depression?
No. While they share symptoms like fatigue and mood swings, postpartum thyroiditis causes physical changes: heart palpitations, heat or cold intolerance, hair loss, and weight changes that aren’t explained by stress or sleep deprivation. Depression primarily affects mood, motivation, and emotional well-being. You can have both at the same time, which is why thyroid testing is essential before starting antidepressants.
Can I get postpartum thyroiditis after a miscarriage or abortion?
Yes. Postpartum thyroiditis can occur after any pregnancy loss, including miscarriage, ectopic pregnancy, or elective abortion. The immune system changes similarly after any pregnancy ends, regardless of outcome. If you have risk factors like high TPO antibodies or type 1 diabetes, testing is recommended within 12 weeks after the event.
Will my baby be affected if I have postpartum thyroiditis?
No, the condition itself doesn’t directly affect your baby. If you’re taking levothyroxine, the amount passed through breast milk is too small to impact your infant’s thyroid. In fact, treating your hypothyroidism helps ensure you have the energy and health to care for your baby. Untreated thyroid issues can indirectly affect bonding and feeding, so treatment supports both your well-being and your baby’s.
How long does it take to feel better after starting treatment?
If you’re on levothyroxine for hypothyroidism, most women notice improved energy and mental clarity within 2-4 weeks. Full symptom relief can take 6-8 weeks. For hyperthyroid symptoms, beta-blockers like propranolol can ease heart palpitations and tremors within hours to days. Patience is key-thyroid hormone levels take time to stabilize.
Can I prevent postpartum thyroiditis?
You can’t prevent it if you’re genetically predisposed. But if you know you’re at risk-like having type 1 diabetes or high TPO antibodies-you can get tested early. Testing at 10-12 weeks postpartum can catch it before symptoms worsen. Early detection means faster treatment and less suffering. There’s no pill or diet that stops it, but awareness saves time and stress.
Should I get tested before my next pregnancy?
If you’ve had postpartum thyroiditis before, yes. Your risk of recurrence is 40%. Get your TSH and TPO antibodies checked before conceiving. If antibodies are high, your doctor may monitor your thyroid more closely during pregnancy. Untreated thyroid issues during pregnancy can affect fetal brain development, so planning ahead matters.
Is postpartum thyroiditis permanent?
In 70-80% of cases, thyroid function returns to normal within 12-18 months. But 20-30% of women develop permanent hypothyroidism and need lifelong levothyroxine. High TPO antibody levels strongly predict this outcome. Even if you recover, you should have your thyroid checked annually for life, as your risk of future thyroid disease remains elevated.
Can stress cause postpartum thyroiditis?
Stress doesn’t cause it, but it can worsen symptoms. Postpartum thyroiditis is an autoimmune condition triggered by immune system changes after pregnancy-not by emotional stress. However, high stress levels can make fatigue, brain fog, and anxiety feel worse, which may delay diagnosis. Managing stress helps you cope, but it won’t stop the thyroid attack.
What’s the difference between postpartum thyroiditis and Hashimoto’s?
They’re almost identical at the cellular level-both involve TPO antibodies attacking the thyroid. The key difference is timing and outcome. Postpartum thyroiditis occurs only after pregnancy and often resolves. Hashimoto’s is a chronic, lifelong condition that can develop at any time. Many women who have postpartum thyroiditis go on to develop Hashimoto’s later. In fact, some experts believe postpartum thyroiditis is just Hashimoto’s that flares after pregnancy.
Are there any natural remedies or supplements that help?
No supplement can reverse autoimmune thyroid damage. Selenium has been studied for its potential to lower TPO antibodies, but results are mixed and it’s not a substitute for medical treatment. Avoid iodine supplements-they can worsen thyroid inflammation. The only proven treatment is thyroid hormone replacement (levothyroxine) when needed. Focus on sleep, nutrition, and medical care-not unproven remedies.







Comments
Marissa Coratti
November 25, 2025 AT 19:39 PMPostpartum thyroiditis is one of those silent epidemics that gets buried under the myth of "just be grateful you have a healthy baby." The autoimmune mechanism is fascinating-pregnancy induces a Th2-dominant immune shift to tolerate the fetus, and postpartum, the immune system rebounds with a vengeance, often targeting the thyroid due to molecular mimicry between placental and thyroid antigens. This isn't just fatigue; it's a physiological recalibration gone awry, and the two-phase pattern is clinically distinct from Graves’ or Hashimoto’s because of the transient nature and low radioactive iodine uptake. Most OB-GYNs don’t screen for it, and that’s a systemic failure.
Rachel Whip
November 26, 2025 AT 10:49 AMI was misdiagnosed with postpartum depression for six months. My TSH was 12.7. I lost 15 pounds in phase one, then gained 20 back. No one connected the dots until I insisted on thyroid panels. If you’re exhausted, cold, and your hair is falling out in clumps-get tested. It’s a simple blood test. You don’t need to suffer for a year thinking it’s "normal."
Brittany Medley
November 28, 2025 AT 06:33 AMThank you for this. I’m a nurse, and I’ve seen so many new moms dismissed as "just tired." The hyperthyroid phase is so subtle-tachycardia, nervousness, heat intolerance-but often chalked up to anxiety or caffeine. Then the crash hits… and they’re told to "sleep more." It’s heartbreaking. I always recommend TSH, free T4, and thyroid antibodies (TPO) at the 6-week checkup, especially if there’s a history of autoimmune disease. Early detection = faster recovery.
Joe bailey
November 29, 2025 AT 23:44 PMMan I wish I knew this when my wife went through it. She thought she was failing as a mom because she couldn’t get out of bed. We went to three doctors before someone checked her thyroid. Now she’s on levothyroxine and back to herself. Seriously, if you’re reading this and you’re a new mom feeling like a ghost in your own body-go get bloodwork. You’re not broken. Your thyroid is just confused.
Micaela Yarman
November 30, 2025 AT 17:04 PMAs someone who immigrated from a country where postpartum care is culturally embedded-this is why we have traditional healers monitor thyroid symptoms at 40 days postpartum. In my homeland, we drink herbal teas, use warm compresses, and rest for 40 days. No one expects you to "bounce back." Here? You’re expected to host brunches at six weeks. The medical system ignores the body’s need to recalibrate after pregnancy. This isn’t just a disease-it’s a cultural failure.
mohit passi
December 1, 2025 AT 15:47 PMlife is weird sometimes 🤷♂️ one day you're glowing with a newborn, next day you're shivering in a t-shirt while everyone else is sweating... turns out your thyroid threw a tantrum. no shame. just science. 🌱
Aaron Whong
December 1, 2025 AT 15:57 PMThe pathophysiology of postpartum thyroiditis is a textbook example of immune reconstitution inflammatory syndrome (IRIS) in the context of pregnancy-induced immunomodulation. The transient hyperthyroid phase reflects thyrocyte destruction with hormone leakage, not true hyperfunction. The subsequent hypothyroid phase is a consequence of follicular depletion and inadequate de novo synthesis. The fact that 20% develop permanent hypothyroidism suggests a continuum with Hashimoto’s, not a discrete entity. We need to reclassify this as a postpartum autoimmune thyroid dysregulation spectrum.
Sanjay Menon
December 3, 2025 AT 08:55 AMI read this and immediately thought: another wellness influencer pushing "thyroid hacks" while ignoring the real issue-modern motherhood is unsustainable. You’re sleep-deprived, underpaid, and expected to be a perfect human incubator. Of course your thyroid is collapsing. The problem isn’t your gland-it’s a society that treats mothers like disposable batteries.
Cynthia Springer
December 4, 2025 AT 23:48 PMMy TPO antibodies were elevated before pregnancy. I didn’t know that was a red flag. Should women with autoimmune conditions be screened before delivery? Or at least counseled? I only found out I was at risk after I’d already been misdiagnosed for months. I’m not mad-I’m just… wondering why no one told me.
Ezequiel adrian
December 6, 2025 AT 03:07 AMthey don't tell you this because hospitals make more money selling antidepressants than running thyroid panels. 5% of moms get this? more like 30% and they just call it "baby blues". wake up people.
Stephen Adeyanju
December 6, 2025 AT 11:00 AMmy wife went through this and no one cared until she cried in the grocery store because she couldn't lift her baby. then they gave her a pamphlet. we paid 800 out of pocket for the test. the system is broken
james thomas
December 7, 2025 AT 02:46 AMthis is all part of the pharmaceutical agenda. thyroid meds are big business. you don't need levothyroxine-you need to eat more coconut oil and stop being so stressed. the real cause? glyphosate in your water. and the government doesn't want you to know.
Asia Roveda
December 8, 2025 AT 17:08 PMif you're a white American woman with college education and insurance, sure, you'll get tested. but if you're poor, Black, or undocumented? you're just "tired". this article is for the privileged. the rest of us are just supposed to survive.