Phosphate Binder Safety Calculator
How This Tool Works
Enter your kidney disease stage and lab values to determine which antacids are safe for you. This tool helps you avoid dangerous interactions based on your specific condition.
Many people reach for antacids like Tums or Milk of Magnesia when they feel heartburn. It’s quick, cheap, and easy-no prescription needed. But if you have kidney disease, what seems like a harmless fix could be dangerous. Antacids aren’t just for stomach acid anymore. In people with chronic kidney disease (CKD), they’re often used as phosphate binders-medications that stop your body from absorbing too much phosphate from food. But here’s the catch: not all antacids are safe, and using them the wrong way can lead to life-threatening complications.
How Antacids Work in Kidney Disease
Antacids like calcium carbonate, aluminum hydroxide, and magnesium hydroxide were originally designed to neutralize stomach acid. But in kidney disease, their role changed. When your kidneys can’t filter phosphate properly-which happens when your glomerular filtration rate (GFR) drops below 30-40%-phosphate builds up in your blood. High phosphate levels cause weak bones, itchy skin, heart problems, and even death.
That’s where antacids come in. Calcium carbonate and aluminum hydroxide bind to phosphate in your gut, forming a compound your body can’t absorb. It then leaves your body in stool. This is why many nephrologists prescribe calcium carbonate as a first-line phosphate binder for early-stage CKD. But here’s what most patients don’t realize: over-the-counter antacids and prescription phosphate binders are not the same thing, even if they contain the same ingredients.
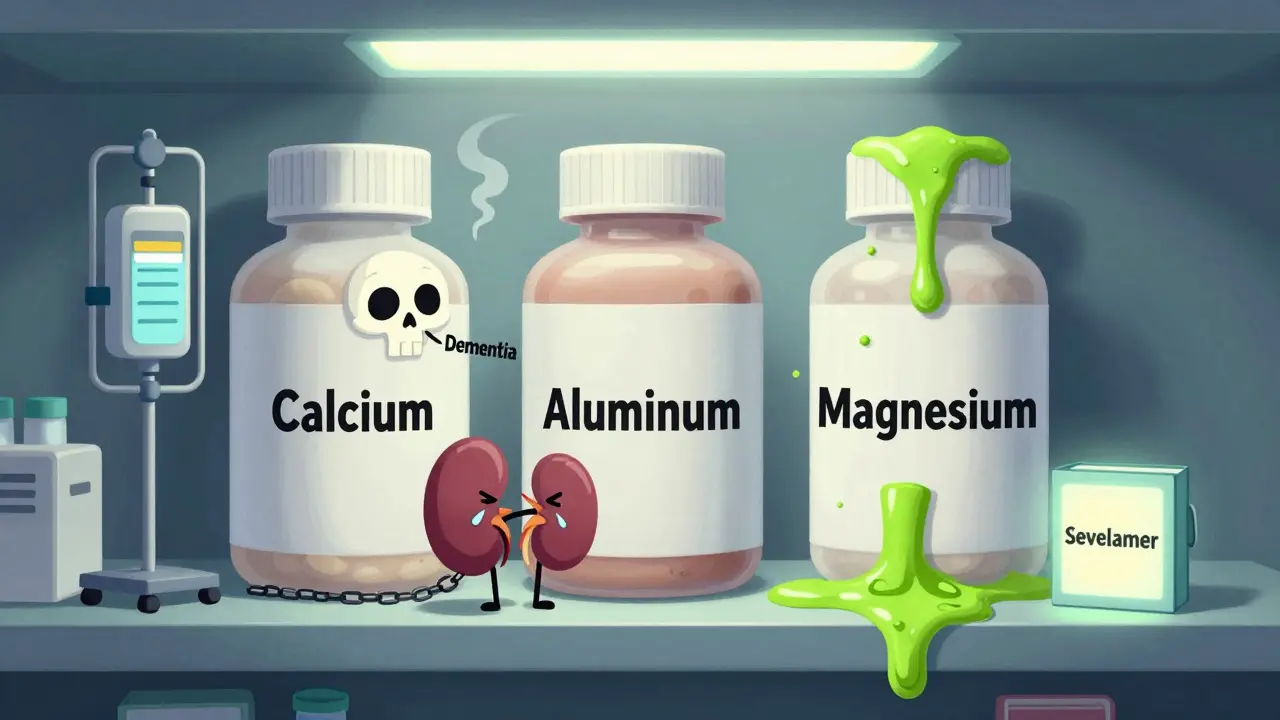
The Three Types of Antacids and Their Risks
Not all antacids are created equal. Each type carries different risks for people with kidney disease.
- Calcium-based antacids (like Tums, Caltrate): These are commonly used because they’re affordable and effective. But in advanced kidney disease, they can cause hypercalcemia-too much calcium in the blood. Levels above 10.2 mg/dL increase the risk of vascular calcification, which hardens arteries and raises the chance of heart attack or stroke. Studies show CKD patients on calcium-based binders have a 30-50% higher risk of cardiovascular events than those on non-calcium alternatives.
- Aluminum-based antacids (like Amphojel, Alu-Cap): These bind phosphate well, but aluminum can build up in your body if your kidneys aren’t working. Even small amounts over time can cause aluminum toxicity. Symptoms include bone pain, dementia-like confusion, muscle weakness, and microcytic anemia. The FDA warns that aluminum levels above 60 mcg/L can cause dialysis dementia. Because of this, aluminum antacids are only approved for short-term use (two weeks max) in people with normal kidneys-and should be avoided entirely in advanced CKD.
- Magnesium-based antacids (like Milk of Magnesia): These are often used for constipation. But in kidney disease, magnesium builds up because your kidneys can’t flush it out. Hypermagnesemia can cause muscle paralysis, low blood pressure, slow heartbeat, and even cardiac arrest. Symptoms start showing when magnesium levels hit 4 mg/dL. In dialysis patients, levels above 10 mg/dL have been fatal.
Prescription Phosphate Binders vs. Over-the-Counter Antacids
Prescription phosphate binders like sevelamer (Renagel), lanthanum carbonate (Fosrenol), and sucroferric oxyhydroxide (Velphoro) were developed specifically for kidney patients. They’re designed to bind phosphate without the dangerous side effects of antacids.
Here’s how they compare:
| Medication | Active Ingredient | Typical Dose per Meal | Phosphate Reduction | Monthly Cost (USD) | Key Risk |
|---|---|---|---|---|---|
| Calcium carbonate (Tums) | Calcium | 1200-1500 mg elemental calcium | 15-25% | $10 | Hypercalcemia, vascular calcification |
| Sevelamer (Renagel) | Polymers | 800-1600 mg | 25-35% | $2,000-2,500 | Gastrointestinal upset |
| Lanthanum carbonate (Fosrenol) | Lanthanum | 750-1500 mg | 25-35% | $2,500-3,500 | GI issues, low iron |
| Sucroferric oxyhydroxide (Velphoro) | Iron-based | 1-2 tablets | 25-30% | $4,000 | Stool discoloration |
| Aluminum hydroxide | Aluminum | 300-900 mg | 20-30% | $15 | Aluminum toxicity, dementia |
| Magnesium hydroxide | Magnesium | 400-1200 mg | 10-20% | $8 | Hypermagnesemia, cardiac arrest |
Prescription binders cost more, but they’re safer. Calcium carbonate is cheaper and works well in early CKD, but it’s risky in stages 4 and 5. Aluminum and magnesium antacids should never be used as long-term phosphate binders. Yet, many patients don’t know the difference.
What the Experts Say
Nephrologists are clear: antacids should never be used as first-line phosphate binders in advanced kidney disease. Dr. Raymond Vanholder, a leading kidney expert in Belgium, says aluminum antacids should be a “last resort” because aluminum damage is irreversible. Dr. Myles Wolf from Duke University recommends calcium carbonate only for CKD stage 3 patients with normal calcium levels-and to stop using it once GFR drops below 30 mL/min.
The National Kidney Foundation warns that magnesium antacids can cause death in stage 4 or 5 CKD patients. A 2022 study from the Mayo Clinic found that 57% of emergency visits related to antacids in kidney patients involved aluminum or magnesium products. Most of these cases happened because patients didn’t know they were at risk.
Real Stories from Patients
On Reddit, one CKD stage 4 patient wrote: “I took Tums every day for heartburn for six months. My nephrologist found my calcium was 11.2 and I had new calcification in my arteries.” Another shared: “I used Milk of Magnesia for constipation and ended up in the ER with magnesium at 8.7. My legs were paralyzed for hours.”
A 2022 survey by the American Association of Kidney Patients found that 68% of CKD patients couldn’t tell the difference between prescription binders and over-the-counter antacids. Forty-two percent had used antacids for heartburn without telling their doctor. While 82% of low-income patients relied on calcium carbonate because insurance wouldn’t cover prescription binders, 35% had been to the ER because of antacid-related problems.

How to Use Antacids Safely with Kidney Disease
If you have kidney disease, here’s what you need to do:
- CKD Stage 3 (GFR 30-59): Calcium carbonate is okay for phosphate control, but only if your calcium levels are normal. Take it with meals. Do not use aluminum or magnesium antacids. Get your calcium, phosphate, and magnesium checked every month.
- CKD Stage 4-5 (GFR <30): Avoid all antacids as phosphate binders. Use only prescription binders under your nephrologist’s care. If you need relief for heartburn, calcium carbonate may be used occasionally-but only if approved by your doctor and taken at least two hours before or after your phosphate binder.
- Always separate antacids from other meds: Antacids can block absorption of antibiotics, thyroid meds, and seizure drugs. Take other medications at least one hour before or four hours after an antacid.
- Know the warning signs: Watch for nausea, confusion, or frequent urination (signs of high calcium); muscle weakness or dizziness (signs of high magnesium); or bone pain and memory issues (signs of aluminum buildup).
What’s Changing in 2025
The FDA now requires stronger warnings on aluminum antacids about kidney risks. Medicare tracks antacid-related hospitalizations in CKD patients as a quality metric. A new drug, tenapanor (Xphozah), was approved in 2023-it works differently by blocking phosphate absorption in the gut without binding it. Early results show fewer side effects.
The NIH is funding a major five-year study called ASK-D, tracking 5,000 CKD patients to create clearer guidelines. Meanwhile, clinics are testing AI tools that personalize phosphate management based on diet, lab results, and genetics.
One thing is certain: the line between “over-the-counter remedy” and “medical treatment” is blurring. What was once a simple fix for heartburn is now a high-stakes decision for millions with kidney disease.
What You Should Do Today
If you have kidney disease:
- Ask your nephrologist: “Am I on a phosphate binder? Is it a prescription drug or an over-the-counter antacid?”
- Check your medicine cabinet. Do you have aluminum or magnesium antacids? If so, stop using them unless your doctor says it’s safe.
- Keep a log: Write down when you take antacids and why. Bring it to your next appointment.
- Don’t assume “natural” or “cheap” means safe. Aluminum and magnesium are natural-but deadly in kidney disease.
Antacids saved lives in the 1950s. Today, they can end them-if used without understanding the risks. Knowledge isn’t just power. In kidney disease, it’s survival.







Comments
Lisa Davies
December 15, 2025 AT 13:37 PMI had no idea Tums could be this dangerous for kidney patients 😱 My mom’s on dialysis and she’s been taking them for years. I’m calling her doctor right now.
Cassie Henriques
December 15, 2025 AT 15:34 PMThe pharmacokinetics here are critical-aluminum’s half-life in CKD is prolonged due to reduced renal clearance, leading to neurotoxic accumulation even at subtherapeutic doses. The FDA’s 60 mcg/L threshold is conservative; some case reports show cognitive decline at 40 mcg/L. This isn’t just about dosing-it’s about bioavailability and cumulative burden.
Nupur Vimal
December 17, 2025 AT 03:09 AMI used Milk of Magnesia for constipation for 3 years and never thought twice about it until my nephrologist told me my magnesium was 7.8 and I was lucky I didn’t have a heart attack. People think natural means safe. It doesn’t. I’m still shaking thinking about it
Jake Sinatra
December 19, 2025 AT 00:16 AMThis is precisely why evidence-based medicine must override over-the-counter convenience. The data is unequivocal: calcium carbonate in Stage 4+ CKD increases cardiovascular mortality by 30-50%. Prescribing OTC antacids without monitoring is malpractice. Patients deserve better than pharmacy aisle solutions.
RONALD Randolph
December 19, 2025 AT 08:50 AMI can’t believe this is even a debate. Aluminum? Magnesium? In kidney patients? Are you kidding me?! These aren’t ‘natural remedies’-they’re slow-acting poisons. The FDA should ban them outright for CKD patients. And stop calling them ‘antacids’-they’re phosphate binders, period. Use the right damn term!
Benjamin Glover
December 20, 2025 AT 00:50 AMThe cost disparity is obscene. $2,500/month for sevelamer versus $10 for Tums. No wonder patients self-medicate. But let’s be honest-most Americans wouldn’t know a phosphate binder if it bit them. This is a systemic failure, not an individual one.
Raj Kumar
December 21, 2025 AT 23:55 PMI’m a CKD patient from India and we don’t even have access to most of these binders. My doc gave me calcium carbonate and told me to take it with meals. I didn’t know there were other options. I’m so glad I read this. I’ll start tracking everything now. Thank you for sharing this.
Melissa Taylor
December 23, 2025 AT 04:22 AMThis is the kind of info that saves lives. Seriously. I’m sharing this with every kidney group I’m in. You’re not being dramatic-you’re being lifesaving. Keep speaking up like this.
John Brown
December 23, 2025 AT 15:30 PMI used to work in a dialysis clinic. Saw too many patients come in with aluminum toxicity-confused, weak, trembling. One guy thought he was just taking ‘stomach medicine.’ No one ever explained the difference. This post should be mandatory reading for every CKD patient. Period.
Christina Bischof
December 25, 2025 AT 12:41 PMI just looked in my cabinet and found three bottles of aluminum antacids. I’ve been taking them for heartburn since my diagnosis 2 years ago. I’m throwing them out tonight. Thanks for the wake-up call.
Jocelyn Lachapelle
December 26, 2025 AT 04:02 AMI’m so glad someone finally said this out loud. My mom’s on dialysis and she still takes Tums like candy. I’ve tried talking to her but she says ‘it’s just calcium.’ I’m printing this out and handing it to her with a highlighter. No more guessing.
Mike Nordby
December 27, 2025 AT 08:53 AMThe NIH’s ASK-D study will be pivotal. If they can correlate genetic polymorphisms in phosphate transporters with binder efficacy and toxicity, we could move toward personalized phosphate management. This isn’t just clinical-it’s precision medicine in action. The data will change guidelines.