When you’re prescribed a blood thinner-whether it’s warfarin, apixaban, rivaroxaban, or dabigatran-you’re told it’s to prevent strokes or clots. But few patients are fully prepared for what happens when the medicine works too well. Severe bleeding isn’t rare. It’s one of the most dangerous side effects of these drugs, and it can happen fast. In fact, over half of all major bleeding events occur within the first three months of starting treatment. And if you don’t know the warning signs, you might wait too long to get help.
Why Blood Thinners Cause Severe Bleeding
Blood thinners don’t actually make your blood thinner. They slow down the clotting process. That’s how they prevent dangerous clots in your heart, brain, or legs. But that same mechanism means even a small injury-like bumping your knee or a minor nosebleed-can turn into something serious. The risk isn’t the same for everyone. Older adults, people with kidney problems, or those taking multiple blood-thinning drugs are at much higher risk. A Swedish study found that people over 80 have more than three times the bleeding risk of those under 60. And if you’ve had a bleed before, your chance of another one jumps by over four times.Which Medications Carry the Highest Risk?
Not all blood thinners are equal. Warfarin has been around for decades and requires regular blood tests (INR checks) to make sure you’re in the safe range. If your INR goes too high, your bleeding risk spikes. DOACs-like apixaban, rivaroxaban, and dabigatran-are easier to use because they don’t need routine testing. But they’re not safer overall. The ARISTOTLE trial showed apixaban had the lowest bleeding rate among DOACs at 2.13% per year, compared to warfarin’s 3.09%. Rivaroxaban and dabigatran had slightly higher rates. Surprisingly, many bleeding events happen in patients on low-dose regimens. One 2024 study found that 58% of bleeding cases occurred in people taking reduced doses, often because doctors thought they were being cautious. But lower doses don’t always mean safer-especially if the drug builds up in the body due to kidney issues.Red Flags: When Bleeding Becomes an Emergency
You don’t need to lose a lot of blood to be in danger. The problem is internal bleeding, which doesn’t always show up right away. Here’s what you need to watch for:- Black, tarry stools (sign of GI bleeding)
- Bloody or dark red urine
- Nosebleeds lasting more than 10 minutes
- Vomiting blood or material that looks like coffee grounds
- Coughing up blood
- Sudden, severe headache or vision changes (possible brain bleed)
- Unexplained bruising, especially large patches or bruises without injury
- Joint swelling or pain after a minor bump
- Excessive menstrual bleeding
- Dizziness, weakness, or feeling faint
One patient on Reddit described how he ignored black stools for three days before ending up in the ER with a bleeding ulcer and needing two units of blood. He didn’t think it was serious until he was dizzy. That’s the trap. Bleeding doesn’t always look like a gushing wound. Sometimes, it’s quiet. And by the time you feel weak or dizzy, you’ve already lost a lot of blood.
Who’s Most at Risk?
Some factors make bleeding far more likely:- Age 75+: Bleeding risk doubles or triples after 75.
- Chronic kidney disease: Poor kidney function means drugs stay in your system longer. This increases bleeding risk by more than two times.
- Previous bleeding event: If you’ve had a GI bleed, brain bleed, or major bruising before, your chance of another one is much higher.
- Taking aspirin or NSAIDs: Even low-dose aspirin can double your bleeding risk when combined with a DOAC.
- High drug levels: Some people naturally metabolize these drugs slowly. A 2024 study showed patients with the highest blood levels of DOACs had over three times the risk of bleeding in the first 90 days.
Doctors use a tool called HAS-BLED to assess your risk before starting treatment. A score of 3 or higher means you need extra monitoring, clearer instructions, and possibly a different medication. If your doctor didn’t go over this with you, ask for it.
What to Do If You’re Bleeding
If you notice any of the red flags above, don’t wait. Don’t call your GP and hope it goes away. Go to the emergency room. Time matters. A 2023 survey found that 37% of people who had major bleeding waited over two hours before seeking help. Nineteen percent waited six hours or more. That delay can be deadly.Here’s what to do immediately:
- Stop any activity. Lie down if you feel dizzy.
- Apply pressure to external wounds. But don’t try to stop internal bleeding-this isn’t something you can fix at home.
- Bring your medication list. Include the name, dose, and time of your last dose.
- Don’t take more medication. Don’t skip doses either-just stop until you’re evaluated.
- Call 999 or go straight to A&E. Tell them you’re on a blood thinner and suspect a bleeding emergency.
Emergency teams have reversal agents ready. For dabigatran, they can give idarucizumab. For rivaroxaban or apixaban, they can use andexanet alfa. These drugs can reverse the anticoagulant effect within minutes. But they’re expensive-up to $12,500 per dose-and not available everywhere. That’s why getting to a hospital fast is critical.
How to Prevent Bleeding Before It Starts
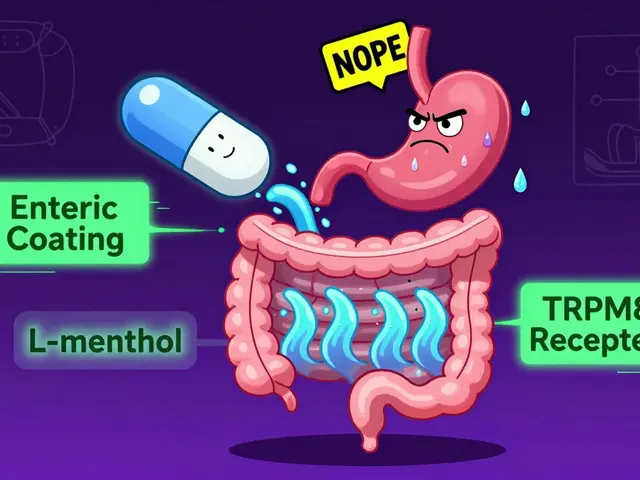
Prevention starts before you even take your first pill:- Get a full kidney function test before starting any DOAC. If your creatinine clearance is below 50 mL/min, your dose may need to be lowered.
- Ask your doctor if you really need a blood thinner. For some older patients with low stroke risk, the bleeding risk may outweigh the benefit.
- Avoid NSAIDs like ibuprofen or naproxen. Use paracetamol instead for pain.
- Use an electric razor. Avoid sharp objects. Be careful with knives and scissors.
- Wear medical alert jewelry. It could save your life if you’re found unconscious.
- Get a bleeding risk assessment (HAS-BLED score) at your first appointment.
Patients who received a 15- to 20-minute education session on bleeding symptoms were 34% less likely to delay emergency care. That’s not just advice-it’s a proven way to reduce deaths.
The Future: Better Tools, Safer Drugs
New developments are coming. In January 2024, the FDA approved the first point-of-care test that can measure DOAC levels in minutes-no lab needed. This means clinics can check your drug levels just weeks after you start treatment and adjust your dose before you bleed. Trials are also underway for new anticoagulants like milvexian and asundexian, which appear to reduce bleeding risk by 20-25% while still preventing clots. And a universal reversal agent called Ciraparantag is in late-stage testing. If it works, it could reverse any blood thinner in one shot.But right now, the best tool you have is knowledge. Know your drug. Know your risk. Know the signs. And if something feels wrong-don’t second-guess yourself. Go to the hospital. Your life depends on it.
Can I stop my blood thinner if I’m worried about bleeding?
No. Stopping your blood thinner without medical supervision can cause a stroke or clot, which can be just as deadly as bleeding. If you’re concerned, talk to your doctor. They can assess your risk, check your drug levels, or switch you to a safer option. Never stop on your own.
Do all blood thinners cause bleeding the same way?
No. Warfarin requires regular INR monitoring and interacts with food and other drugs. DOACs like apixaban and rivaroxaban have fixed doses and fewer interactions, but they’re cleared by the kidneys. If your kidneys aren’t working well, the drug builds up and increases bleeding risk. Apixaban has the lowest bleeding rate among DOACs, especially for GI bleeding.
How long does it take for bleeding to become life-threatening?
It can happen in minutes to hours. Internal bleeding, like a brain or stomach bleed, may not cause pain right away. But as blood loss continues, you’ll feel weak, dizzy, or confused. Once your blood pressure drops, organs start to shut down. The faster you get treatment, the better your chance of survival. Waiting even an hour can make a difference.
Can I still exercise or play sports while on blood thinners?
Yes-but avoid high-risk activities. Swimming, walking, cycling, and light strength training are generally safe. Avoid contact sports like football or boxing. Be cautious with activities that could cause falls or head injuries, like skiing or rock climbing. Always wear protective gear, and tell your coach or trainer you’re on a blood thinner.
Are there natural alternatives to blood thinners?
No. Supplements like garlic, ginger, fish oil, or vitamin E may have mild blood-thinning effects, but they’re not strong enough or reliable enough to prevent strokes or clots. Relying on them instead of prescribed medication puts you at serious risk. If you want to reduce your need for blood thinners, focus on managing your underlying condition-like atrial fibrillation-with your doctor’s help.
What should I tell emergency staff when I arrive?
Tell them: 1) You’re on a blood thinner, 2) The name and dose of the drug, 3) When you last took it, 4) What symptoms you’re having, and 5) That you’re worried about bleeding. Bring your medication bottle or list. This helps them act quickly-especially if you’re unable to speak.






Comments
Dusty Weeks
January 1, 2026 AT 19:55 PMthis is wild. i took apixaban for afib and ignored a nosebleed for 20 mins. thought it was just dry air. turned out i lost a quarter of my blood volume. ER saved me. dont be me.
Sally Denham-Vaughan
January 3, 2026 AT 17:19 PMi love how doctors just hand out these drugs like candy. no one tells you the real risks. my uncle died from a brain bleed on rivaroxaban. they said it was "unpredictable." bull. it was predictable if you actually listened.
Richard Thomas
January 4, 2026 AT 14:09 PMthere's something deeply human about how we treat medicine as a binary. take it or don't. safe or dangerous. but life isn't like that. blood thinners are a negotiation with mortality. every pill is a quiet bet that your body won't betray you. and when it does, the silence before the collapse is the worst part. not the blood. not the pain. the quiet. the assumption that this time, it'll be fine.
sharad vyas
January 5, 2026 AT 09:24 AMin india, many elders take aspirin with warfarin because they think it helps heart. no one tells them it doubles bleeding risk. my aunt almost died. now i carry a printed sheet in hindi for my family. knowledge is the only vaccine.
Phoebe McKenzie
January 6, 2026 AT 20:51 PMTHIS IS WHY WE NEED TO STOP LETTING PHARMA COMPANIES CONTROL OUR HEALTH. DOACS ARE A SCAM. THEY’RE MORE EXPENSIVE, LESS MONITORED, AND MORE LIKELY TO KILL YOU IN SILENCE. WARFARIN IS OLD BUT AT LEAST YOU KNOW WHERE YOU STAND. THEY WANT YOU DEPENDENT. THEY WANT YOU AFRAID. THEY WANT YOUR MONEY.
gerard najera
January 7, 2026 AT 04:47 AMHAS-BLED score is underused. Ask for it.
Paul Ong
January 8, 2026 AT 16:07 PMdont wait till youre dizzy go now if you see black stool or weird bruising no excuses i saw a guy pass out in the parking lot of walmart from internal bleed he was fine because he called 911 right away
Andy Heinlein
January 10, 2026 AT 13:56 PMi was scared to take my blood thinner after reading this but then i remembered my dad had a stroke at 68. so i take it. and i wear my medical alert bracelet. and i tell my kids what to do if i collapse. knowledge + action = peace of mind 🙏
Todd Nickel
January 10, 2026 AT 16:18 PMthe 2024 study showing 58% of bleeding events occurred on reduced doses is profoundly counterintuitive. it suggests that clinical caution, particularly in elderly or renally impaired patients, may inadvertently increase risk due to pharmacokinetic accumulation. this undermines the assumption that lower doses are inherently safer and highlights the necessity of therapeutic drug monitoring even in "low-risk" regimens. the disconnect between intention and outcome here is alarming.
Austin Mac-Anabraba
January 11, 2026 AT 20:11 PMyou people are being manipulated. the FDA approved these DOACs because they’re more profitable. warfarin is cheap. it’s been around for 70 years. they don’t want you on it. they want you on the $12,000 reversal agents and monthly co-pays. the bleeding stats are real-but the system is rigged. don’t be a lab rat.
Stephen Gikuma
January 12, 2026 AT 01:28 AMthis is all part of the globalist medical agenda. why do you think they push these drugs? so you get sick, go to the hospital, and then they track you with your ID bracelet. next thing you know, they’re injecting you with microchips through the IV. they don’t care if you bleed. they care if you’re controlled.
Bobby Collins
January 13, 2026 AT 12:50 PMi think the government is putting something in the water to make people need blood thinners. why else would so many old people be on them? my neighbor’s husband started one after he drank tap water for 30 years. coincidence? i think not.
Liam George
January 14, 2026 AT 00:28 AMthe systemic failure here is structural. pharmaceutical incentives prioritize market expansion over physiological precision. DOACs were engineered for convenience, not safety. the absence of routine monitoring creates a false sense of security. Meanwhile, renal clearance variability-especially in aging populations-is treated as an edge case rather than a clinical imperative. The current paradigm assumes uniform metabolism. Biology doesn't comply. The result? Predictable chaos. We need population-level pharmacokinetic screening before prescribing, not after the bleed.
Ann Romine
January 15, 2026 AT 19:06 PMi work in a rural clinic. we don’t have andexanet alfa. we don’t even have a full lab. when a patient bleeds, we give them vitamin K, fresh frozen plasma, and pray. the fact that reversal agents exist but aren’t accessible to half the country is a moral crisis. this isn’t just medical-it’s justice.
Bill Medley
January 17, 2026 AT 18:45 PMThe data presented is compelling and aligns with current clinical guidelines. Immediate emergency response remains the most critical intervention. Prevention through risk stratification and patient education is both effective and underutilized. Further dissemination of HAS-BLED assessment and point-of-care testing should be prioritized in primary care settings.