When a pill says it expires in June 2025, most people think, "I’ll just toss it then." But for some medications, that date isn’t just a suggestion-it’s a line between life and death. This is especially true for drugs with a narrow therapeutic index (NTI). These aren’t your average painkillers or antihistamines. They’re powerful, precise tools used to treat serious conditions like heart failure, epilepsy, bipolar disorder, and blood clots. And if they lose even a little bit of potency after expiration, the consequences can be deadly.
What Exactly Is a Narrow Therapeutic Index?
A narrow therapeutic index means there’s almost no room for error. The difference between a dose that works and a dose that harms is tiny-sometimes less than 20%. Think of it like driving a car where the gas pedal only works in a 1-inch range. Press too lightly, and you stall. Press too hard, and you crash. The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in blood concentration can cause serious side effects, therapy failure, or even death. For example:- Warfarin (a blood thinner): A 10% drop in potency might mean your blood doesn’t thin enough, leading to a stroke or pulmonary embolism. A 10% increase could cause uncontrolled bleeding.
- Digoxin (for heart rhythm): The safe range is 0.5 to 0.9 ng/mL. Above 1.2 ng/mL, you risk fatal heart arrhythmias. That’s less than a 33% increase from safe to toxic.
- Lithium (for bipolar disorder): Blood levels must stay between 0.6 and 1.0 mEq/L. Above 1.5, you get tremors, confusion, seizures-even coma.
- Phenytoin (for seizures): Too low, and seizures return. Too high, and you lose coordination, develop slurred speech, or suffer liver damage.
Why Expiration Dates Matter More for NTI Drugs
Every medicine has an expiration date. That’s the last day the manufacturer guarantees the drug will work as intended-under proper storage conditions. For most drugs, a small drop in potency might not matter. A 10% weaker ibuprofen still helps with a headache. But for NTI drugs, that same 10% drop can push you out of the therapeutic window. Take warfarin again. If a tablet loses 10% of its strength after expiration, and you’re taking 5 mg daily, you’re now getting only 4.5 mg. That might sound small. But for someone with a mechanical heart valve, that drop could push their INR (a blood clotting measure) from 2.8 down to 2.2. Suddenly, they’re no longer protected from clots. The risk of stroke skyrockets. And it’s not just about losing strength. Some drugs break down into toxic byproducts. Tetracycline, for example, turns into a kidney-damaging compound when expired. While not an NTI drug, it shows how degradation isn’t always harmless. For NTI drugs, we don’t know all the breakdown products-but we know even small changes are dangerous. The FDA’s standards for generic NTI drugs prove how precise these medications need to be. For most drugs, generics must be 80-125% as potent as the brand-name version to be approved. For NTI drugs like levothyroxine, phenytoin, and tacrolimus, the acceptable range is much tighter: 90-111%. That’s ±11%, not ±25%. Why? Because a 15% difference in potency could be fatal. If a drug degrades just 5% past its expiration date, that’s already more than half the allowed variation under FDA bioequivalence rules. That’s not a minor issue. That’s a clinical emergency waiting to happen.Real-World Consequences of Using Expired NTI Medications
There are no large-scale studies tracking expired NTI drugs in real patients-mostly because no one should be taking them. But we know what happens when potency shifts. A 2014 study in the Journal of Clinical Pharmacy and Therapeutics found that drug-related problems involving NTI medications were far more likely to cause hospitalization or permanent injury than those involving other drugs. Why? Because small errors have big effects. Consider this real case: A 68-year-old man on digoxin for atrial fibrillation took a bottle of pills he’d had for two years past the expiration date. He felt fine-no symptoms. But his blood level came back at 1.4 ng/mL. Toxic. He was rushed to the hospital with a dangerously slow heart rate. He survived. But only because his doctor caught it. Another patient on lithium for bipolar disorder switched to a generic brand that was slightly less potent. His mood stabilized. Then he used an old bottle of his previous brand-expired by eight months. He didn’t realize the pills were different. Within days, he became confused, shaky, and vomited. His lithium level was 1.8 mEq/L. He needed emergency dialysis. These aren’t rare. They’re predictable. And they’re preventable.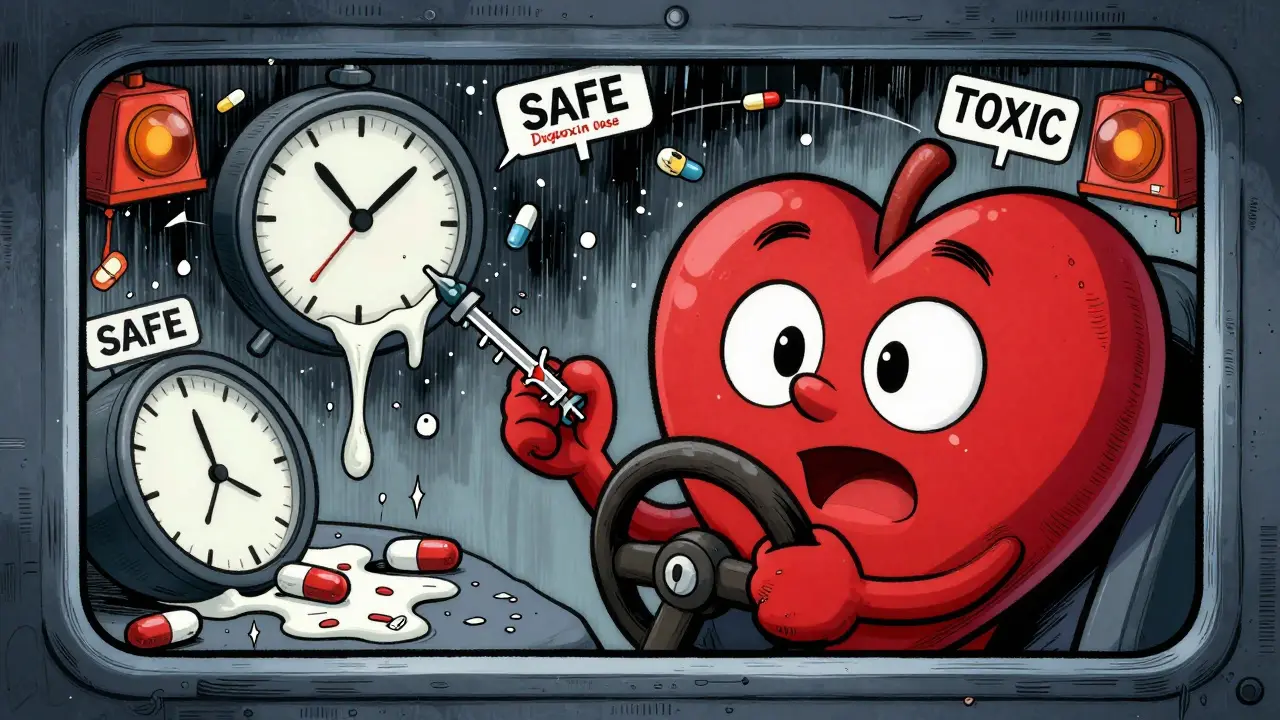
What Healthcare Providers Should Do
Doctors, pharmacists, and nurses are on the front lines. They need to treat NTI drugs as high-alert medications-like insulin or heparin. The Institute for Safe Medication Practices (ISMP) says exactly that: treat them with extra caution. Here’s what they should do:- Never dispense expired NTI drugs-even if they look fine. Storage conditions matter. Heat, humidity, and light degrade pills faster than you think.
- Ask patients if they’re using old prescriptions. Many keep them “just in case.”
- Use electronic alerts in pharmacy systems to flag NTI drugs with expired dates.
- Document substitutions carefully. Switching from one brand of levothyroxine to another-even if both are generic-can change absorption and require a dose adjustment.
- Teach patients to check expiration dates every time they refill. Don’t assume the pharmacy checked.
What Patients Need to Know
If you take an NTI drug, here’s your simple rule: Never use it after the expiration date. Don’t rely on the myth that “medicines last forever.” The FDA says most drugs retain 90% potency for years past expiration-if stored perfectly. But that’s not the same as safe or effective for NTI drugs. Even 5% degradation is too much. Here’s what to do:- Write down your drug’s expiration date and set a reminder 30 days before it expires.
- Don’t refill early just to stockpile. NTI drugs need fresh batches. Your body is sensitive to even slight changes.
- Return expired meds to a pharmacy take-back program. Don’t flush them or throw them in the trash.
- Never share your pills. Even if someone has the same diagnosis, their dose is tailored to them.
- Ask your pharmacist: “Is this a narrow therapeutic index drug?” If they don’t know, ask your doctor.
What’s Being Done-and What’s Not
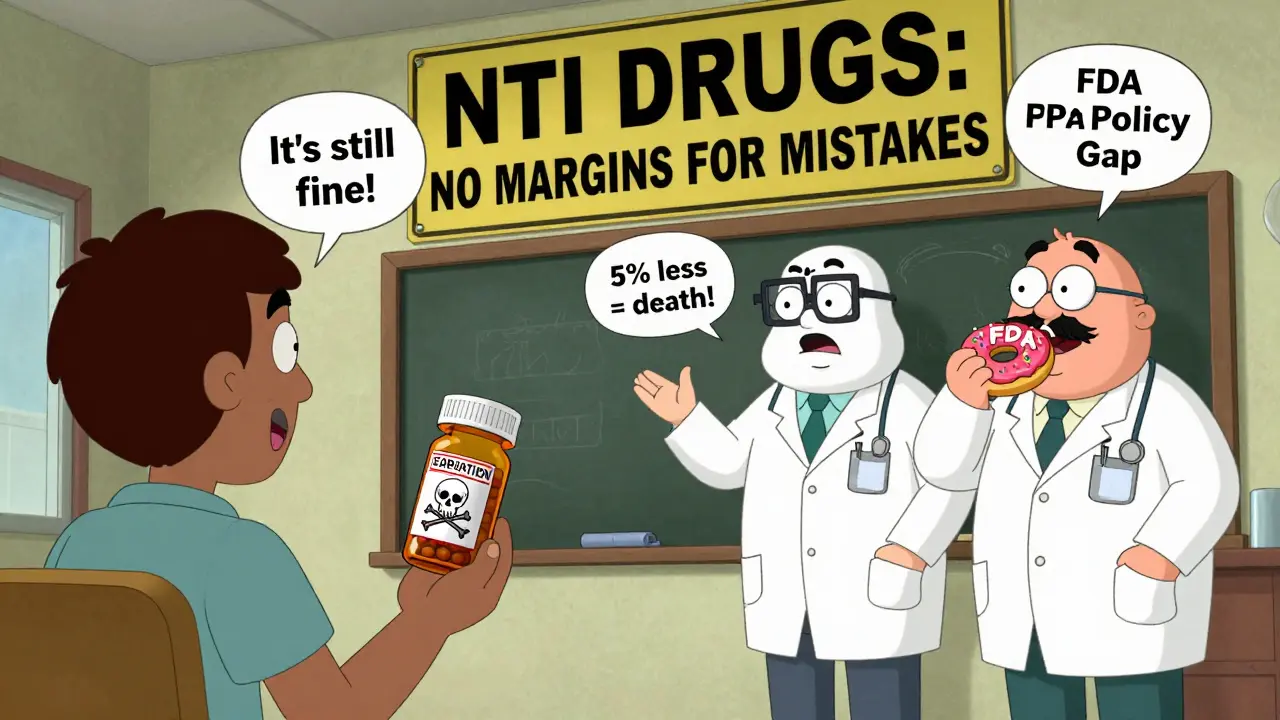
The FDA has taken steps. Since 2011, they’ve required stricter bioequivalence testing for NTI drugs. Manufacturers now use advanced methods to ensure consistency. Some are even testing stability beyond expiration dates-78% of major drugmakers now do extended testing for critical NTI products. But here’s the gap: There are no official guidelines on expiration dates for NTI drugs. The FDA hasn’t said, “These drugs must be discarded 6 months after expiration.” They haven’t required special labeling. They haven’t mandated refrigeration or light-proof packaging for all NTI drugs. The European Medicines Agency recognizes the risk-but hasn’t acted either. Professional groups like the American Pharmacists Association are calling for change. They want specific expiration warnings on NTI drug packaging. They want training for pharmacists. They want public education. Until then, the responsibility falls on you and your care team.Bottom Line: When in Doubt, Don’t Take It
Expiration dates aren’t arbitrary. For most drugs, they’re conservative. For NTI drugs, they’re life-or-death thresholds. If you’re on warfarin, lithium, digoxin, phenytoin, or any other NTI medication:- Check the date every time you refill.
- Never take a pill past its expiration-even if it looks fine.
- Call your doctor or pharmacist if you’re unsure.
- Dispose of expired drugs safely.
What drugs have a narrow therapeutic index?
Common NTI drugs include warfarin, lithium, digoxin, phenytoin, carbamazepine, levothyroxine, tacrolimus, cyclosporine, aminoglycosides (like gentamicin), theophylline, and phenobarbital. These require precise dosing and regular blood monitoring because small changes in concentration can cause serious harm or treatment failure.
Can expired NTI drugs still be safe if they look fine?
No. Appearance doesn’t indicate potency. Pills can degrade without changing color, smell, or texture. For NTI drugs, even a 5% loss in strength can push blood levels out of the safe range. The risk isn’t worth taking.
Is it okay to use an expired NTI drug in an emergency?
Never. If you’re out of your NTI medication, contact your doctor or go to an emergency room. Using an expired dose can lead to stroke, seizure, heart failure, or death. There are no safe exceptions.
Why don’t expiration dates for NTI drugs have special labels?
Currently, the FDA doesn’t require special expiration labeling for NTI drugs. This is a gap in safety policy. While manufacturers test stability, no federal rules mandate shorter expiration dates or warning labels. Professional organizations are pushing for change, but as of 2026, patients must assume all NTI drugs are time-sensitive.
How can I tell if my medication is an NTI drug?
Ask your pharmacist or doctor directly. You can also look up your drug on the FDA’s website or in DrugBank. If your doctor checks your blood levels regularly (like INR for warfarin or lithium levels), it’s almost certainly an NTI drug. Don’t guess-ask.