When you walk into a doctor’s office for a new prescription, who really gets to decide what goes into your body? It’s not just the doctor’s call. Not anymore. The truth is, medication autonomy - your right to choose, question, and even refuse a drug - is now a core part of modern healthcare. But it’s not always practiced the way it should be.
Why Your Choice Matters More Than You Think
Think about it: you wouldn’t let someone force you to eat food you’re allergic to, or wear clothes that make you uncomfortable. So why should you be told to take a pill you don’t want, just because a doctor says it’s ‘best’? Medication isn’t like a bandage you stick on and forget. It changes how you feel, how you sleep, how you move through your day. Some cause nausea. Others zap your energy. A few affect your sex life, your mood, even your weight. These aren’t side effects - they’re life changes. That’s why autonomy isn’t just ethical. It’s practical. Studies show that when patients help choose their meds, they stick with them 82% of the time. When the doctor picks alone? That number drops to 65%. You’re more likely to take something you helped pick. Simple as that.What Does Real Autonomy Look Like?
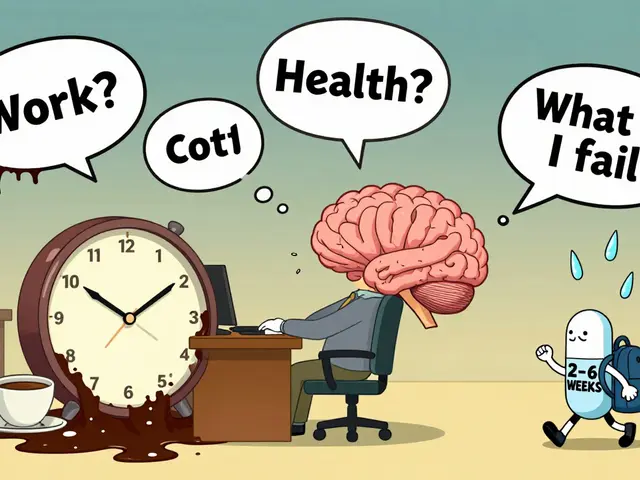
Autonomy doesn’t mean saying ‘yes’ or ‘no’ to a script. It means having a real conversation. A good clinician will walk you through:- What the drug actually does - not just ‘it helps depression,’ but how it works in your brain
- How likely it is to work for you - for example, SSRIs help about half of people with major depression
- What the side effects really are - like sexual dysfunction, which happens in 25-30% of users
- What alternatives exist - including cheaper generics, non-drug options like therapy, or even different delivery methods (patches, liquids, once-daily pills)
- How much it costs - because if you can’t afford it, you won’t take it, no matter how good it is
The Gap Between Theory and Practice
You’d think this is standard by now. But it’s not. Only 45% of primary care doctors consistently use shared decision-making for medications. Compare that to 68% for surgery - where the stakes are higher. Why the difference? Time. Most appointments last 15 minutes. That’s not enough to unpack your fears, your budget, your past bad experiences with meds. And it’s worse in rural areas. Only 42% of clinics in underserved communities even try. Meanwhile, in big hospitals, electronic records often don’t have fields to even record your preferences. Only 38% of Epic systems - used by 78% of U.S. hospitals - let you document what you want. That means your choice gets lost before it’s even written down.
Cost Isn’t Just a Number - It’s a Decision
Here’s the raw truth: if a drug costs $6,000 a month and you’re on Medicare, you’re not choosing based on science. You’re choosing based on whether you can afford to eat next month. In 2023, 32% of Medicare Part D users changed or skipped doses because of cost. That’s not noncompliance - that’s survival. And it’s not just about brand names. Biosimilars - cheaper versions of biologic drugs - can save you $2,000 a month. But many doctors don’t bring them up unless you ask. Why? Because they assume you won’t understand. Or worse - they assume you can’t afford to care.Who’s Really in Control?
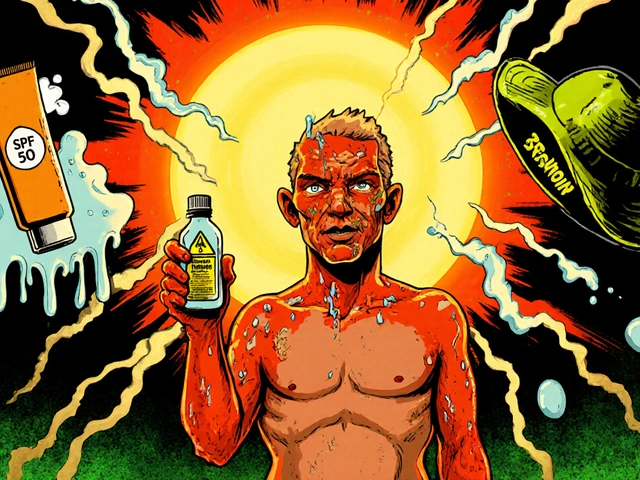
Pharmaceutical ads play a role too. In 2023, 28% of patients asked for a drug because they saw it on TV. That’s not necessarily bad - but it’s not informed. You might hear about a new weight-loss pill, but not hear about the 1 in 5 people who get pancreatitis. That’s why the FDA now tracks these requests. And why some experts warn: when patients choose based on marketing, they’re not exercising autonomy. They’re being marketed to. Then there’s the cultural side. Immigrant patients, Black and Hispanic communities, older adults - they’re less likely to feel empowered to question a doctor. A 2023 survey found only 49% of Black patients felt involved in medication decisions, compared to 74% of white patients. That’s not a gap in knowledge. It’s a gap in trust - and in how care is delivered.Real Stories, Real Choices
One cancer patient refused opioids because of her religious beliefs. Her doctor didn’t push. They built a pain plan with nerve blocks, physical therapy, and non-opioid meds. She stayed in control. She stayed comfortable. Another patient with diabetes was prescribed Ozempic but felt sick just thinking about the nausea. Her doctor said, ‘It’s the best option.’ She switched providers. The new one sat down with her, showed her alternatives - including GLP-1 alternatives with fewer GI side effects - and helped her pick one that fit her life. She’s been on it for six months now. No vomiting. No regret. These aren’t rare cases. They’re what autonomy looks like when it works.
How to Take Back Your Power
You don’t need a degree in medicine to be an active participant. Here’s how to start:- Before your appointment, write down: What do I want this medication to do? What am I afraid of? What have I tried before?
- Ask: ‘Are there other options - cheaper, simpler, or with fewer side effects?’
- Ask: ‘What happens if I don’t take this?’ Sometimes the answer is ‘nothing serious’ - and that’s valuable.
- Ask: ‘Can I try this for a month and reassess?’ Many drugs can be tested short-term.
- Ask for written materials or apps that explain your options. Mayo Clinic and the CDC have free, plain-language guides.
The Future Is Personal
The next big shift? Personalized medicine. In 2024, a full genetic test that tells you how your body processes drugs costs just $249 - down from $1,200 in 2020. That means your doctor could soon say, ‘Based on your genes, this drug will likely make you sick. Try this one instead.’ Digital tools are coming too - apps that help you weigh pros and cons, track side effects, and even simulate what life would be like on each option. But here’s the catch: 37% of people over 65 can’t use them. If we don’t fix that, autonomy becomes a privilege for the tech-savvy - not a right for everyone.It’s Not About Saying No. It’s About Saying Yes - on Your Terms
Medication autonomy isn’t about rejecting medicine. It’s about owning your health. It’s saying: ‘I trust you, but I also trust myself.’ The system still has holes. Doctors are rushed. Records don’t talk to each other. Ads muddy the waters. But the power is yours - if you know how to use it. You have the right to ask. To pause. To compare. To say, ‘Let me think about this.’ You have the right to walk out and find someone who’ll listen. Because in the end, no one lives your life but you. And no one should decide what goes into your body - except you, with the facts, the support, and the respect you deserve.Can I refuse a prescription even if my doctor insists on it?
Yes. If you have decision-making capacity - meaning you understand the risks, benefits, and alternatives - you have the legal and ethical right to refuse any medication, even if your doctor disagrees. Doctors can explain why they recommend a drug, but they cannot force you to take it. This is protected under informed consent laws established in the U.S. since the 1972 Canterbury v. Spence case. Some doctors may try to pressure you, but you can request a second opinion or switch providers.
What if I can’t afford my prescribed medication?
Cost should never be a hidden barrier. Ask your doctor for generic alternatives, patient assistance programs, or biosimilars - which can cost up to 40% less than brand-name drugs. Many pharmaceutical companies offer coupons or free trials. You can also ask your pharmacist about discount programs like GoodRx. If you’re on Medicare, you can apply for Extra Help to lower drug costs. If your doctor refuses to discuss affordability, it’s a red flag - you deserve a provider who treats cost as part of the medical decision.
How do I know if I’m truly making an informed choice?
You’re making an informed choice if you understand: what the drug does, how likely it is to work for you, what side effects you might face, what alternatives exist, and how it fits into your daily life. If your doctor doesn’t explain these points clearly, ask for written materials or use trusted resources like the Mayo Clinic’s decision aids. If you feel rushed or pressured, you’re not getting full information. Pause the conversation. Schedule a follow-up. Your choice should feel clear, not confusing.
Can I change my mind after starting a medication?
Absolutely. Medication decisions aren’t permanent. Many drugs need to be tried for weeks before you know if they work - but if side effects are unbearable or you realize it doesn’t fit your life, you can stop. Always consult your doctor before stopping, especially for antidepressants or blood pressure meds, but your right to discontinue remains. In fact, 50% of people with chronic conditions stop their meds within a year - often because they didn’t feel involved in the initial choice. Don’t feel guilty for changing your mind. Feel empowered.
Why do some doctors seem resistant to discussing medication options?
Some doctors are overwhelmed, undertrained, or operating in systems that don’t reward time spent on shared decisions. Others may assume you won’t understand, or that you’ll pick the cheapest option - and that’s a bias, not a fact. Studies show patients who are involved in decisions have better outcomes. If your doctor dismisses your questions, says ‘trust me,’ or acts annoyed, it’s not you - it’s the system. You have every right to find a provider who respects your role in your care.




Comments
Angel Tiestos lopez
January 14, 2026 AT 09:44 AMbro this is the most real thing i’ve read all year 🙏 i’ve been on 3 different antidepressants and none of them felt like *me*... finally found one that didn’t turn me into a zombie. my doctor didn’t push. just asked what i wanted to feel. that’s all i needed. 🌱
Trevor Davis
January 15, 2026 AT 15:15 PMI appreciate the thoughtful framing of this piece. It's not merely about patient rights-it's about dignity in healthcare. The data supporting shared decision-making is overwhelming, and yet, systemic inertia persists. We must demand structural reform, not just individual empowerment.
mike swinchoski
January 16, 2026 AT 21:30 PMYou people are ridiculous. Doctors know best. If you don't take your meds, you're just a lazy hypochondriac. My grandma took her pills even when she felt fine and she lived to 92. Stop being so dramatic.
Damario Brown
January 17, 2026 AT 22:32 PMlol so u wanna 'autonomy' but u cant even spell 'pharmaceutical' right? 😂 also 82% adherence? where'd u get that? that's not a real study. it's probably from some pharma-funded think tank. and don't even get me started on 'biosimilars'-they're basically generics with a fancy name. you think you're woke but you're just gullible.
sam abas
January 18, 2026 AT 23:39 PMOkay but let’s be real-this whole ‘patient autonomy’ thing is just a distraction. The real issue is that the healthcare system is broken. You think asking your doctor ‘what are the alternatives?’ is gonna fix $6,000/month drugs? Nah. You need to fix insurance, fix drug pricing, fix the fact that doctors get paid to prescribe, not to educate. Autonomy is a Band-Aid on a hemorrhage. And don’t even get me started on those ‘decision aids’-half the time they’re written in 12th-grade reading level and assume you own a smartphone. Most of my cousins over 60 still use flip phones. So yeah, autonomy? More like privilege.
John Pope
January 20, 2026 AT 04:03 AMThe system is a goddamn theater. We’re all actors in a play written by Big Pharma and the AMA. You think you’re choosing? Nah. You’re being nudged. The ‘shared decision-making’ checklist? It’s a script. The doctor reads line 3, you say line 4, they nod, you sign. The real power? It’s in the algorithm that decides which drug pops up first in the EHR. That’s not autonomy. That’s algorithmic coercion. And the worst part? We all play along because we’re too tired to fight. 🎭💊
Clay .Haeber
January 22, 2026 AT 01:58 AMOh wow. So now we’re giving people the power to make life-or-death decisions based on what they saw on a TikTok ad about Ozempic? Brilliant. Next we’ll let them pick their chemotherapy based on Yelp reviews. 🙃 The irony? The people screaming loudest about ‘autonomy’ are the same ones who think a $249 genetic test will solve everything. Meanwhile, the guy in rural Alabama can’t even get a prescription filled because the pharmacy is 40 miles away. Autonomy? More like performative woke capitalism.
Priyanka Kumari
January 22, 2026 AT 10:52 AMThis is exactly what healthcare should be. I’m from India, and in my village, elders never question doctors-it’s seen as disrespectful. But my cousin, who has diabetes, finally found a provider who sat with her for an hour, showed her the numbers, asked what she wanted her life to look like. She switched to insulin pens, started walking daily, and now her HbA1c is stable. It wasn’t magic. It was respect. We need more of this-not less. Thank you for writing this.
Avneet Singh
January 23, 2026 AT 21:44 PMThe entire premise is flawed. Autonomy presupposes cognitive capacity, which is not universally distributed. Many patients lack health literacy, financial means, or even access to the internet. To frame this as a moral imperative is to ignore structural inequity. It’s not about empowerment-it’s about placing the burden of systemic failure on the individual. The real solution? Universal healthcare with mandated physician training in shared decision-making. Not ‘ask your pharmacist.’