Every year, Americans fill over 4 billion prescriptions. Nine out of ten of those are for generic drugs. Yet, many doctors still reach for the brand-name version-sometimes without even realizing it. Why? Because medical schools rarely teach them how generics actually work.
What Bioequivalence Really Means
When a generic drug hits the market, it doesn’t just copy the brand name. It has to prove it delivers the same active ingredient, in the same amount, at the same speed, and to the same place in the body. That’s called bioequivalence. The FDA requires that the average absorption rate (AUC) and peak concentration (Cmax) of the generic fall within 80% to 125% of the brand drug’s numbers. That’s not a guess. It’s based on studies with 24 to 36 healthy volunteers, measured with lab-grade precision.
But here’s the catch: most doctors never learn what those numbers mean. In medical school, pharmacology courses spend hours on how Lipitor lowers cholesterol, but less than 30 minutes on how a generic version of atorvastatin does the exact same thing. The science is solid. The training isn’t.
Why Doctors Still Doubt Generics
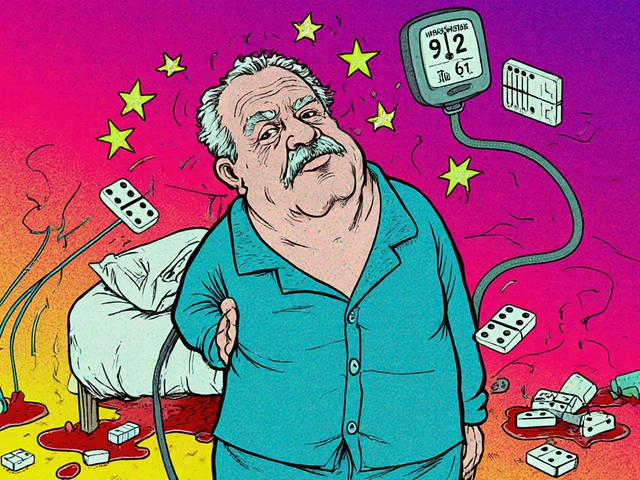
It’s not about distrust in regulators. It’s about lived experience. In 2016, a few patients on generic methylphenidate (the active ingredient in Concerta) reported their ADHD symptoms returned. The FDA investigated. The generics met all bioequivalence standards. But patients still felt different. Doctors noticed. And they remembered.
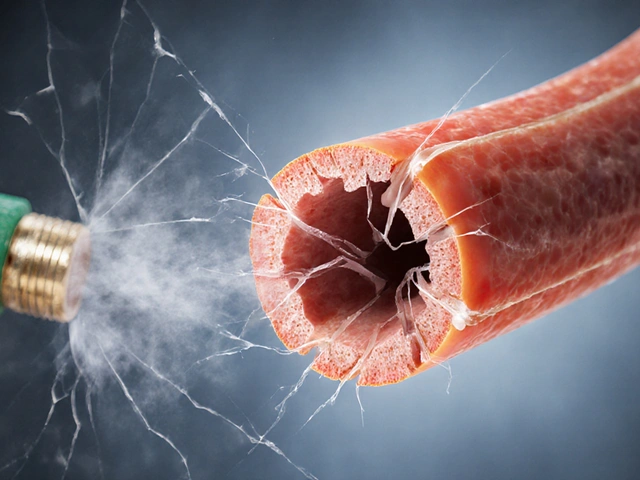
That incident didn’t break the system-it exposed a gap. When a patient says, “This generic doesn’t work like the brand,” and the doctor doesn’t have a clear, science-backed answer, they default to what’s familiar: the brand. Especially when treating conditions with narrow therapeutic windows-like epilepsy, warfarin, or levothyroxine. In a 2022 survey, nearly a quarter of neurologists admitted they avoid switching patients to generics for seizure meds, even though the FDA says the same standards apply.
It’s not irrational. It’s human. If your training never taught you how to explain why a 10% difference in absorption doesn’t matter for most drugs, you’ll err on the side of caution. Especially when you have 15 seconds to decide on a prescription.
What Medical Schools Aren’t Teaching
A 2023 analysis by the Association of American Medical Colleges found that 78% of case studies in medical textbooks still use brand names. Students learn about “Advair,” not “fluticasone/salmeterol.” They memorize “Zoloft,” not “sertraline.” By the time they’re prescribing, the brand name is the default. The generic? Just an afterthought.
And it’s not just naming. Medical schools rarely teach how to interpret bioequivalence data. They don’t show students how to read a pharmacokinetic curve. They don’t explain why a 10% difference in Cmax is meaningless for a statin but might matter for a blood thinner. They don’t train them to ask: “Is this a simple molecule or a complex delivery system?”
At Karolinska Institute in Sweden, they fixed this in 2018. They made International Nonproprietary Names (INN) mandatory in all prescriptions written by students. Graduates started prescribing generics 47% more often. No lectures. No handouts. Just a rule: write the generic name. And it stuck.
What Actually Changes Behavior
Knowledge alone doesn’t change prescribing habits. A 2015 study in Malaysia gave 30 doctors a 45-minute lecture on generics. Their knowledge scores jumped from 58.7% to 84%. But their prescribing didn’t budge. Why? Because they still heard their senior colleagues say, “Use the brand.” Culture beats curriculum.
What does work? Feedback loops. The Nature Scientific Reports study found that pharmacists who reviewed 100 prescriptions with feedback improved their understanding by 40%. The same principle applies to doctors. When a system gives you real-time feedback-“This patient was switched to generic metformin. Their HbA1c dropped from 8.2 to 7.1. No adverse events”-you start to trust the data.
Another winner? The teach-back method. Instead of saying, “This generic is just as good,” ask the patient: “Can you tell me why we’re switching?” If they can explain it, you know they understand. In one family practice, this cut patient questions about generics by 63%. It’s not about convincing. It’s about confirming.
Technology Can Help-If It’s Designed Right
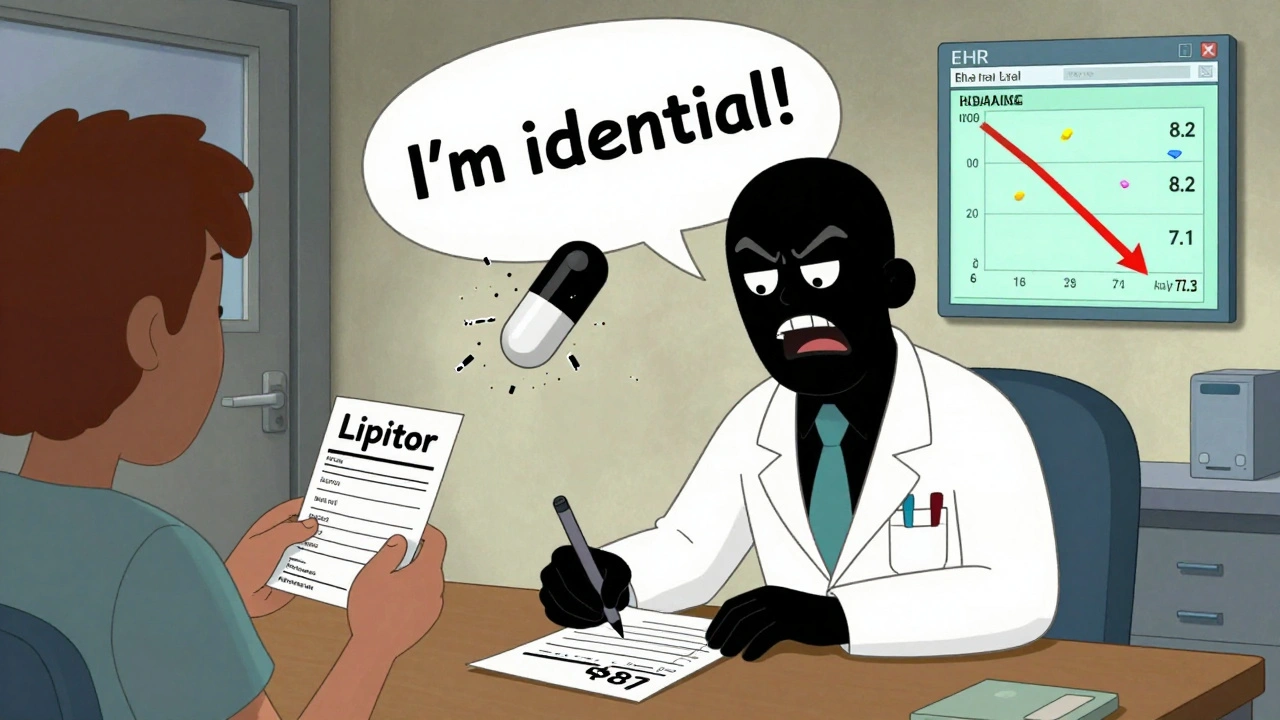
Electronic health records (EHRs) could be the game-changer. Right now, only 38% of U.S. healthcare systems have decision-support tools that flag when a generic is available and show bioequivalence data at the point of prescribing. Imagine this: you type in “Lipitor.” The system pops up: “Generic atorvastatin available. Bioequivalent. Saves $87/month. 92% of patients maintain same lipid levels.” That’s not a suggestion. That’s a nudge backed by evidence.
The FDA’s Digital Health Center of Excellence is building exactly that. By late 2025, bioequivalence data will be integrated directly into EHRs. No more Googling. No more guessing. Just one click to see the science.

Why This Matters Beyond the Prescription
Generics make up 90% of prescriptions but only 22% of drug spending. That’s $156 billion in potential savings by 2030-if doctors prescribe them confidently. But savings don’t happen if patients don’t trust them. A 2024 Kaiser Family Foundation poll found 38% of U.S. adults worry about generic drug quality. Why? Because their doctor never explained it.
When a doctor says, “This is the same medicine, just cheaper,” patients hear: “This is the cheap version.” But when a doctor says, “This version has been tested in 30 people to make sure it works just like the brand. The FDA requires it. And here’s what the data shows,” patients feel respected. They’re more likely to fill the script. And stick with it.
What’s Changing-And What’s Not
The FDA launched a new initiative in 2023: 15-minute microlearning modules on bioequivalence for providers. Free. Online. Accessible. They cover the science, the myths, and the real-world data. But adoption? Only 28% of providers report using them. Why? Because they’re optional. And doctors are overwhelmed.
Real change comes from structure. Mandatory INN prescribing in training. Feedback on every generic switch. EHR alerts that show real outcomes. Integration into licensing exams. These aren’t fancy ideas. They’re basic professional standards-like handwashing or double-checking allergies.
And yet, only 43% of U.S. teaching hospitals have formal generic drug education resources. That’s not an oversight. It’s a system failure.
The Bottom Line
Doctors don’t need more lectures. They need better tools, better feedback, and better training that starts on day one of medical school. Generics aren’t second-rate. They’re science-tested, cost-saving, life-changing. But they won’t be prescribed unless doctors are taught to believe in them-not just know about them.
The data is clear. The science is solid. The savings are massive. What’s missing is the curriculum. And until that changes, doctors will keep reaching for the brand. Not because they’re wrong. But because they were never shown the right way.




Comments
John Biesecker
December 2, 2025 AT 23:43 PMbro i just realized i’ve been taking generic lisinopril for 3 years and my blood pressure is better than when i was on the brand 😅 maybe the FDA knows more than my doc who still says 'brand is safer'... but like... why do we still do this?
Genesis Rubi
December 3, 2025 AT 17:14 PMgeneric drugs are for peasants. real medicine comes in fancy packaging with a logo. if you can't afford the brand you shouldn't be sick. america is built on quality not cheap shortcuts. 🇺🇸
Doug Hawk
December 4, 2025 AT 22:57 PMthe bioequivalence window is 80-125% but nobody talks about the variance in excipients. that’s where the real clinical variability hides. i’ve seen patients crash after switching generics because of filler sensitivity. it’s not the active ingredient-it’s the delivery matrix. medical schools ignore this entirely. and yeah, the data says it’s fine... but medicine isn’t just data. it’s lived experience. and patients feel it.
John Morrow
December 5, 2025 AT 05:26 AMthe entire argument rests on the assumption that bioequivalence translates to therapeutic equivalence, which is a fallacy. pharmacokinetics are not pharmacodynamics. the FDA’s standards are statistically derived from small, homogenous populations-healthy young adults. real patients have comorbidities, polypharmacy, renal impairment, hepatic variations. the 10% difference in Cmax? That’s not meaningless-it’s the difference between seizure control and status epilepticus. And no, you don’t get that from a 30-minute lecture. You get it from 12 years of clinical trauma.
Kristen Yates
December 5, 2025 AT 10:26 AMI’ve been a pharmacist for 22 years. I’ve seen people cry because they couldn’t afford their brand. I’ve seen them refill generics and say, 'I feel like myself again.' It’s not magic. It’s science. But we have to stop making people feel guilty for choosing the cheaper option.
Saurabh Tiwari
December 5, 2025 AT 12:10 PMin india we use generics every day and no one cares. if it works it works. why make it complicated? 🤷♂️
Michael Campbell
December 6, 2025 AT 23:12 PMthe FDA is in bed with Big Pharma. they let generics in so the drug companies can keep making profits. you think they want you to save money? nah. they want you hooked on the system. trust no one.
Victoria Graci
December 8, 2025 AT 14:56 PMit’s wild how we treat medicine like it’s a cult. we worship brand names like they’re sacred incantations. 'Lipitor' sounds like a spell. 'Atorvastatin' sounds like a typo. we’ve trained ourselves to believe that if it doesn’t have a catchy name, it’s not real. but the molecule doesn’t care what you call it. it just does its job. maybe the problem isn’t the drug… it’s the story we tell ourselves.
Saravanan Sathyanandha
December 9, 2025 AT 16:23 PMIn many developing countries, generics are the backbone of public health. Without them, millions would go untreated. The science is not debatable-it is replicated across continents, languages, and systems. The resistance is cultural, not clinical. We must reframe the narrative: generics are not inferior. They are equitable. And equity in medicine is not a luxury-it is a right.
Fern Marder
December 10, 2025 AT 15:18 PMyou people are so naive. if generics were truly equivalent, why do they cost 90% less? because they’re cheaper. because they’re worse. don’t be fooled by FDA jargon. your life isn’t a statistic.
Saket Modi
December 11, 2025 AT 05:54 AMwhy are we even talking about this? just let the doctors do their thing. i’m just here for the memes.
Chris Wallace
December 12, 2025 AT 18:14 PMthe Karolinska example is the only real solution. mandatory INN prescribing. no exceptions. no debates. just force the habit. because knowledge doesn’t change behavior-environment does. if the EHR auto-fills the generic, if the prescription pad only has INNs printed on it, if the student is graded on using the generic name… then the culture shifts. not because they believe it, but because they have no other option. that’s how habits form. not through lectures. through systems.
Sheryl Lynn
December 13, 2025 AT 13:06 PMthe fact that we’re even having this conversation proves how broken medical education is. we teach students to memorize 2000 drug names, 90% of which are brand names, then wonder why they don’t prescribe generics. it’s like teaching someone to drive by only showing them the logo on the hood of a Ferrari. they’ll never recognize a Toyota. and then they blame the driver when they crash.
ruiqing Jane
December 15, 2025 AT 04:22 AMwe need to stop treating patients like they’re incapable of understanding science. when we say 'this is the same medicine, just cheaper,' we’re not just being lazy-we’re disrespecting them. teach them the data. show them the curves. let them see the studies. let them ask questions. when they understand, they become allies. and when patients advocate for generics, doctors listen. it’s not about convincing doctors. it’s about empowering patients.