When you’re prescribed a biologic therapy, you’re not just getting a new drug-you’re taking on a new responsibility. These powerful medications, used for conditions like rheumatoid arthritis, psoriasis, and Crohn’s disease, come in pens or syringes you’re expected to use at home. But if you haven’t been trained properly, a simple injection can turn into a serious risk. Biologic therapy injection isn’t just about pushing a button. It’s about cleanliness, confidence, and consistency-and missing any of those can lead to infection, treatment failure, or even hospitalization.
Why Injection Training Isn’t Optional
You’d think if a doctor gives you a biologic, they’d make sure you know how to use it. But the truth is, many patients get a 30-minute demo and are sent home with a box of pens. A 2022 study found that while 92% of patients say they received training, the average session lasted just 30 minutes. That’s not enough. Real training isn’t watching someone else do it. It’s doing it yourself-over and over-until it’s automatic. The FDA requires manufacturers to provide training materials, but there’s no standard for how it’s delivered. Some clinics use videos. Others hand you a pamphlet. Only about 27% of patients get the full package: tell (explanation), show (demonstration), and try/do (hands-on practice). Without all three, you’re flying blind. And the consequences? One in three patients report feeling unsure about their technique within the first month. By six months, over a third still lack confidence. That’s not just stress-it’s a safety gap. Poor technique is linked to a 37% higher risk of skin infections, according to CDC guidelines.How Infections Start (And How to Stop Them)
Biologics suppress your immune system. That’s how they help with autoimmune diseases. But it also means your body can’t fight off germs as easily. A tiny break in your skin-like a nick from a dirty needle or an unclean injection site-can become an infection that spreads fast. The most common mistakes that lead to infection:- Not washing hands properly before handling the pen
- Using alcohol wipes that dry too quickly without full contact time
- Reusing needles or syringes (never do this)
- Injecting over a mole, scar, or bruised area
- Not rotating injection sites, leading to tissue damage
What Real Training Looks Like
Good training isn’t a one-time event. It’s a process. Studies show that spreading training over three short sessions-each 15 to 20 minutes-boosts retention by 62% compared to cramming it all into one visit. Here’s what effective training includes:- Hands-on practice with a trainer device-these look and feel like your real pen but contain no medicine. Use it until you can activate it without looking.
- Teach-back method-your nurse or pharmacist asks you to explain each step in your own words. If you can’t, they reteach. This works 3.2 times better than just listening.
- Video review-many manufacturers now offer apps with short videos you can watch before each injection. Adbry and other brands have virtual coaching built in.
- Emotional prep-anxiety causes 57% of early treatment dropouts. Simple breathing techniques, a set time of day, or a ritual (like playing a song or lighting a candle) help reduce fear.
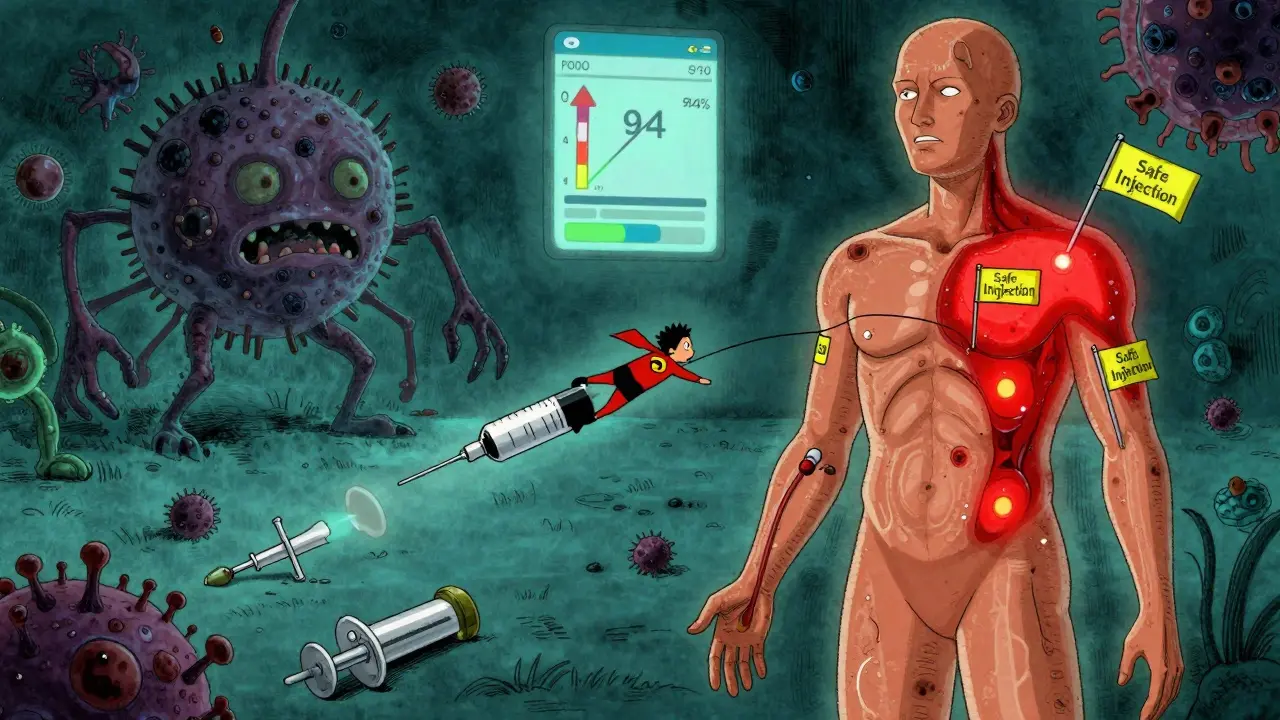
- Follow-up visits-patients who had three or more supervised injections retained proper technique at 94% after six months. Those with only one session? Only 52%.

Why Your Environment Matters
You’re not in a clinic anymore. You’re on your couch. In the bathroom. At 11 p.m. after a long day. That’s when mistakes happen. The Rheumatologist reports that 68% of injection errors occur during the first 10 home injections. Why? Distractions. Fatigue. Lack of light. No clean surface. Create a dedicated injection space. Pick a quiet, well-lit spot. Keep your supplies in one place: pens, alcohol wipes, sharps container, tissue. Wash your hands. Wipe the surface. Use a clean towel. Don’t inject in the kitchen if you’ve just handled raw meat. Don’t do it in the car. Don’t rush. Use the "breathing room" trick: if you’re nervous, have someone gently place their hand over yours during the injection. It stops you from jerking the pen away too soon. It’s simple. It works.What to Do If You Mess Up
You drop the pen. You see blood. You think you didn’t inject deep enough. You panic. Here’s what not to do: Don’t re-use it. Don’t try to inject again in the same spot. Don’t ignore redness or swelling. If you’re unsure whether the dose was delivered:- Don’t inject another dose. You could overdose.
- Call your pharmacy or clinic. They’ll tell you what to do.
- Keep the used pen. They may need to check the mechanism.
The Bigger Picture: Training Is Broken-But Fixable
The global biologics market is projected to hit $331 billion by 2027. More people are using these drugs than ever. But only 38% of healthcare providers have access to standardized training protocols. That’s not just a gap-it’s a crisis. Patients are being set up to fail. And the system knows it. The FDA released new draft guidance in March 2023 pushing for consistent, structured training. Some companies are stepping up: digital platforms now offer video tutorials, reminders, and even AI feedback on injection technique. But until every clinic, every pharmacy, every provider adopts a minimum standard, you have to be your own advocate. Ask for more than a demo. Ask for practice. Ask for follow-up. Ask for help with anxiety. You deserve to feel safe with your treatment.Final Checklist: Before Every Injection
- ✅ Wash hands for 20 seconds with soap and water
- ✅ Use a clean, dry surface
- ✅ Check expiration date and liquid clarity
- ✅ Clean injection site with alcohol wipe, wait 30 seconds to dry
- ✅ Rotate site by at least 1 inch from last injection
- ✅ Use trainer device if unsure about technique
- ✅ Dispose of needle in sharps container immediately
- ✅ Note site and time in log
Can I reuse my biologic injection pen or needle?
No. Biologic pens are designed for single use only. Reusing needles or pens increases your risk of infection, clogging, and inaccurate dosing. Even if the needle looks clean, bacteria can hide in tiny crevices. Always use a new pen or needle for each injection.
What should I do if I accidentally inject into a vein?
Biologic injections are meant for subcutaneous tissue, not veins. If you see blood in the syringe or pen, stop immediately. Do not inject. Remove the device and discard it safely. Contact your healthcare provider for guidance. Do not attempt another injection until you’ve spoken with them. Injecting biologics into a vein can cause serious reactions.
How do I know if my injection site is infected?
Signs of infection include redness larger than 2 cm (about the size of a quarter), warmth to the touch, swelling, pus, or increasing pain. You may also develop a fever over 100.4°F (38°C). If you notice any of these, call your doctor right away. Don’t wait. Biologics weaken your immune response, so infections can spread quickly.
Why do I feel so anxious about injecting myself?
It’s completely normal. Most people feel nervous about needles, especially when they’re injecting a powerful medication. The key is to create a routine: same time, same place, same ritual-like playing calming music or taking a deep breath before each injection. Practice with a trainer device until it feels automatic. Many patients find that once they’ve done it 5-10 times, the fear fades. If anxiety persists, ask your provider about counseling or support groups.
Can my pharmacist help me with injection training?
Yes-often better than your doctor. Pharmacists are trained in medication counseling and have more time to walk you through each step. Many offer free injection coaching, including practice with trainer pens, video resources, and follow-up calls. Ask your pharmacy if they have a patient support program. Don’t wait until you’re confused-reach out early.
What if I forget my injection schedule?
Set phone reminders for each injection day. Many biologic manufacturers offer free apps that send alerts, track your sites, and even show video tutorials. If you miss a dose, don’t double up. Check the medication guide or call your pharmacy for instructions. Consistency matters more than perfection. Missing one dose won’t ruin your treatment, but skipping regularly can reduce its effectiveness.






Comments
Harriet Hollingsworth
December 31, 2025 AT 02:51 AMLet me get this straight-you’re expected to inject life-altering drugs at home with zero real training? This isn’t healthcare, it’s negligence wrapped in a pamphlet. I’ve seen people bleed out from a dirty needle because they were told to "just wing it." Someone needs to get sued. This is criminal.
And don’t even get me started on the "alcohol wipe for five seconds" nonsense. You wouldn’t scrub a toilet that fast. Why are we scrubbing skin like it’s a dirty dish?
My aunt died from a biologic infection because they didn’t teach her to rotate sites. Don’t tell me this is "normal." It’s not. It’s a death sentence with a side of corporate profit.
Retha Dungga
January 1, 2026 AT 06:34 AMlife is a needle 🧵💉 and we’re all just trying not to poke our eyes out 😅 but seriously… wash your hands like your life depends on it… because it does. 🙏 #biologicwarrior
Jenny Salmingo
January 2, 2026 AT 20:17 PMI know how scary this is. I’ve been on biologics for 4 years. The first time I did it, I cried. I thought I’d mess up and hurt myself. But I made a little ritual-play my favorite song, sit in my comfy chair, light a candle. Now it’s just part of my day.
Don’t beat yourself up if you’re nervous. You’re not broken. You’re brave. And you’re not alone. I’ve got your back.
Brandon Boyd
January 2, 2026 AT 23:55 PMListen. You’re not a patient. You’re a warrior. Every time you pick up that pen, you’re choosing to fight. And you’re doing it right. No one handed you a trophy for this. You earned it.
Here’s the truth: you don’t need perfect technique-you need consistent effort. Miss a day? No biggie. Forgot to rotate? Just fix it next time. You’re not a machine. You’re human. And humans get messy.
But here’s the win-you’re still here. Still doing it. That’s more than most. Keep going. I believe in you.
Branden Temew
January 4, 2026 AT 21:12 PMSo let me get this straight-we’ve got a $331 billion industry that’s literally betting on people not knowing how to use a needle… and they call it "healthcare?"
It’s like giving someone a rocket ship and saying, "Here, go to Mars. We’ll send you a PDF."
And the saddest part? The people who actually need this stuff are too tired, too scared, or too broke to demand better. So we just… keep injecting.
Brilliant. Truly. The future is bright.
…I’m gonna go cry now.
Frank SSS
January 6, 2026 AT 17:02 PMOkay, real talk-I read this whole thing and I’m exhausted. Not because it’s long. Because it’s *true.*
I’ve been doing this for 3 years. I’ve had two infections. I’ve cried in the bathroom after botching an injection. I’ve used the same alcohol wipe twice because I was too tired to get up.
And guess what? No one asked me how I was *feeling.* They just handed me the pen and said, "You got this."
So yeah. I’m not mad. I’m just… tired. And I wish someone had told me it was okay to be tired.
Marilyn Ferrera
January 6, 2026 AT 23:40 PMWash hands for 20 seconds. Alcohol wipe for 30 seconds. Rotate sites. No reusing. Track everything. This is non-negotiable. If you skip one step, you’re gambling with your health. Period.
Robb Rice
January 8, 2026 AT 11:38 AMAs someone who’s been on biologics since 2018, I can say this: training matters. I got mine from my pharmacist-free, 45 minutes, hands-on with a dummy pen. I still use the app they gave me.
But I’ve seen others… just wing it. And it’s scary. I wish more clinics would partner with pharmacies. They’re the real unsung heroes here.
Also, I misspelled "alcohol" in my notes once. It was embarrassing. But I learned. You will too.
Stewart Smith
January 9, 2026 AT 19:37 PMYeah… I get it. You’re supposed to be a perfect little injection robot. But sometimes, you’re just… tired. And the lights are flickering. And your kid is crying. And you’re holding the pen like it’s a grenade.
And that’s okay.
You don’t have to be flawless. You just have to show up. And you’re showing up. That’s enough.
Aaron Bales
January 11, 2026 AT 00:18 AMPharmacists are your secret weapon. Seriously. They know the drug inside out. They’ve trained hundreds of people. They don’t have a 10-minute appointment slot. They have time.
Walk in. Say: "I need help with my injection technique." No apology. No excuse. Just ask. They’ll help. And if they don’t? Find one who does.
You deserve this. Demand it.
Lawver Stanton
January 12, 2026 AT 16:38 PMLet me tell you about the time I injected into my belly button because I was watching TikTok. Yeah. That happened. I didn’t even notice until the next day when my skin looked like a sunset.
And guess what? No one called me out. No one asked if I was okay. Just a new pen and a pamphlet.
So here’s my hot take: the whole system is designed to make you feel guilty for being human. But you’re not broken. The system is.
And I’m not even mad. I’m just… disappointed. Like, deeply. Like when you buy a phone that says "waterproof" and it dies in the rain.
Same energy.
Sara Stinnett
January 14, 2026 AT 00:27 AMHow dare you suggest this is a "safety gap"? This is a systemic failure of capitalism masquerading as medicine. You think they care if you get an infection? No. They care if you keep buying the $10,000 vial every month.
Training? Handouts? Video tutorials? These are PR stunts. They’re not meant to help you-they’re meant to shield them from lawsuits.
And you? You’re just a revenue stream with a needle.
Wake up. You’re not a patient. You’re a product.
…I’m sorry. I didn’t mean to be harsh. But someone has to say it.
linda permata sari
January 15, 2026 AT 17:41 PMI am from Indonesia. I never thought I would need this. But now I do. I cried when I first injected. My husband held my hand. We watched the video three times. I wrote down every step in my notebook.
Now I do it every Tuesday at 7 p.m. with my favorite tea. I am not afraid anymore.
Thank you for writing this. I feel less alone.