Drug Interactions: Simple Tips to Stay Safe When You Mix Medications
Ever wonder why your doctor warns you about certain drug combos? It’s not just extra paperwork – mixing meds can change how they work, cause unexpected side effects, or even make you sick. Understanding the basics helps you protect yourself without needing a medical degree.
Why Interactions Happen
Most drugs travel through the same pathways in your body, especially the liver and kidneys. When two medicines use the same pathway, they can compete, slowing down or speeding up each other’s effects. For example, an antibiotic might block the breakdown of a blood‑thinner, raising the risk of bleeding. Another common case: an over‑the‑counter pain reliever can raise the level of a heart medication, causing a rapid heartbeat.
Quick Ways to Spot Dangerous Mixes
1. Keep a Master List. Write down every prescription, over‑the‑counter pill, vitamin, and herb you take. Update the list whenever a doctor adds or removes something.
2. Ask Before You Add. Before buying a new OTC product or supplement, check it against your list. A quick chat with your pharmacist can catch hidden interactions.
3. Watch the Timing. Some meds are safe if taken several hours apart. For instance, calcium supplements can lower the absorption of certain antibiotics if you take them together. Spacing them out can solve the problem.
4. Look for Red Flags. Common signs of a bad interaction include sudden dizziness, nausea, unusual bruising, or a rapid heartbeat. If any of these appear after you start a new drug, call your doctor right away.
Remember, not every combo is dangerous – many are perfectly fine. The key is to stay informed and involve your healthcare team.
For extra peace of mind, use reputable drug‑interaction checkers online or ask a pharmacist to run a quick review. It only takes a minute, and it can save you from a nasty surprise later.
Bottom line: a little vigilance goes a long way. Keep your medication list handy, double‑check new additions, and never ignore odd symptoms. Your body will thank you for the extra care.
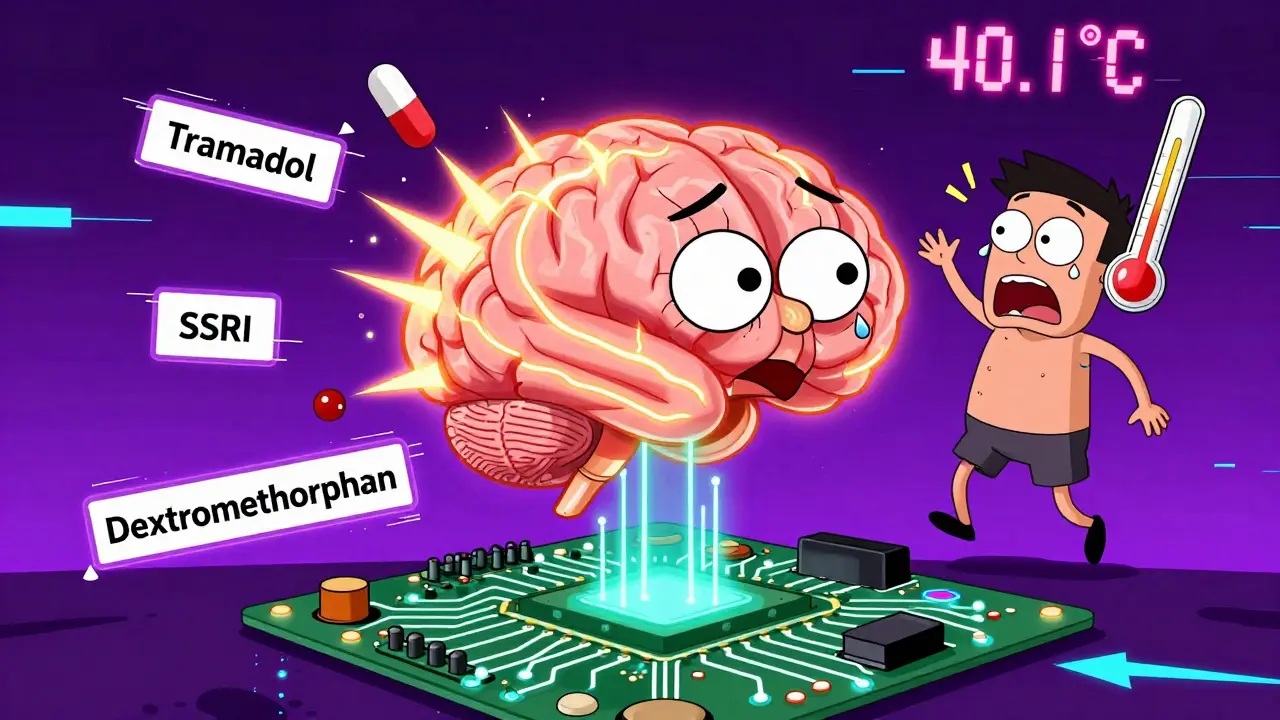
Opioids and Serotonin Syndrome: What You Need to Know About Dangerous Drug Mixes
Certain opioids like tramadol and dextromethorphan can trigger serotonin syndrome when mixed with antidepressants. Learn which painkillers are safe, which to avoid, and what to do if symptoms appear.
St. John’s Wort and Prescription Drug Interactions: What You Must Know
St. John's Wort can make prescription drugs like warfarin, birth control, and antidepressants stop working - with life-threatening results. Learn which medications are at risk and what to do instead.
Bisoprolol Fumarate Interactions: Drug, Food, and Lifestyle Factors You Must Know
Bisoprolol fumarate is a popular medication for managing blood pressure and heart conditions. But did you know certain drugs, foods, and everyday habits can mess with how it works? This article breaks down all the crucial interactions to watch out for, shares some surprising stats, and gives real-world tips for staying safe. Discover which combinations are risky and simple ways to keep your heart in top shape.